Learn more about spinal surgeries and their risks: Spinal Surgeries
آخر تحديث :
Spinal Surgeries
Spinal surgeries are known to be among the most challenging and complex surgical interventions in the field of medicine. The operations conducted by Dr. Amr Amal in the field of spine are exemplary in this regard. He is a skilled surgeon specialized in treating and diagnosing spine problems using the latest surgical techniques. In this article, we will take a look at some of the prominent surgeries performed by Dr. Amr Amal.
- Spinal Fusion Surgery: Spinal fusion surgery is one of the procedures performed in cases of bone fragments or unstable slips in the spine. Dr. Amr Amal anesthetizes the patient and makes an incision in the skin to eliminate this problem and stabilize the affected vertebrae using screws or rods. This procedure helps strengthen the spine’s structure and improve the movement of the damaged vertebrae.
- Diskectomy: In cases where there is pressure on the nerves in the spine due to a slipped disk, Dr. Amr Amal performs a surgical operation in which the damaged disk is removed, relieving the pressure on the nerves. This improves pain and restores normal movement to the vertebrae. This procedure relies on early diagnosis and the use of the latest surgical techniques to ensure the best results.
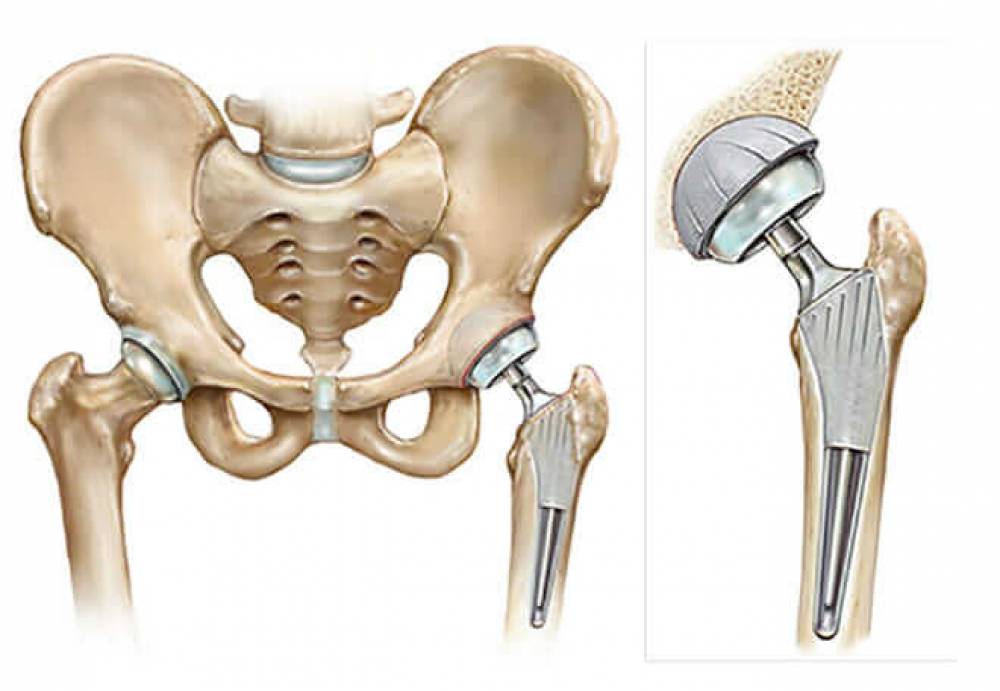
- Joint Replacement Surgery: In cases of damage to the spinal joint due to arthritis or wear and tear, Dr. Amr Amal offers joint replacement surgery. This procedure requires removing the damaged joint and replacing it with an artificial one. This surgery restores flexibility and normal movement to the spine and reduces the pain associated with arthritis.
- Restoring the Spine’s Natural Posture: In cases of spinal deformities such as kyphosis or scoliosis, Dr. Amr Amal offers programs to restore the spine’s natural posture. These programs include muscle training and improving flexibility through physical therapy exercises and corrective braces.
- Removal of Spinal Tumors: In cases of malignant or benign tumors in the spine, Dr. Amr Amal offers surgery to remove spinal tumors. Magnetic resonance imaging is used to determine the location and size of the tumor, and then the surgical operation is performed to remove the tumor and restore the spine’s normal functions.
All these operations and procedures conducted by Dr. Amr Amal are based on surgical precision and the latest technologies. His aim is always to improve the quality of life of the patients and restore the normal movement and functions of the spine. If you are suffering from spine problems, consulting Dr. Amr Amal might be the first step towards recovery.
Are Spinal Surgeries Dangerous?
Many people suffer from spinal problems, and spinal surgeries are a common option for treating some of these issues. But are these surgeries considered dangerous? In this article, we will look at 5 important facts that help us answer this question.
Spinal Surgeries are Surgical Interventions: Spinal surgeries are procedures that require surgical intervention to correct problems in the spine. Of course, undergoing any surgical procedure can pose risks.
The Risk May Vary from Case to Case: The risk associated with spinal surgeries can vary depending on the nature of the problem and its severity. There may be some cases that require complex surgeries and are considerably dangerous, while other cases may involve less risky procedures.
The Ability to Improve Health Condition: Despite the potential risks of spinal surgeries, the primary goal of these procedures is to improve the patient’s condition. The surgery may be necessary to relieve pain, restore mobility, and correct any issues in the spinal inflammation.
Potential Complications: As with any surgical procedure, complications can occur during or after spinal surgeries. Common complications include poor wound healing, excessive infections, internal bleeding, and loss of sensation or movement. However, it should be noted that thanks to advancements in medical technology, the potential risks of these procedures are lower than before.
Preparation and Post-Surgery: Spinal surgeries may require substantial preparation before the procedure and a recovery period afterward. Patients must follow the doctor’s instructions and undergo necessary examinations before the surgery and continue to follow ongoing instructions after the procedure to achieve the best possible outcome and minimize the risks of muscle strain and delayed healing.
In general, it can be said that spinal surgeries are not necessarily dangerous in an absolute sense. The potential benefits should be weighed against the potential risks, and a decision should be made based on specialized medical consultation and a personal assessment of the condition.
What is the Success Rate of Spinal Surgery?
Spinal surgery is one of the surgical procedures aimed at treating spinal issues, such as structural deformities, injuries, and tumors. The success rate of this procedure is one of the main criteria considered by both patients and doctors alike.
It is important to note that the success of spinal surgery depends on numerous factors, including the type and severity of the spinal issue, as well as the surgeon’s experience and skill. In some cases, the patient’s age and overall health condition may also impact the success rate.
Nonetheless, the success rate of spinal surgery is generally considered high. For example, the success rate of spinal disc surgery can reach around 90%, while the success rate of spinal fusion surgeries ranges between 80% and 95%, according to studies and research reports. Many factors influence this rate, including the surgeon’s level of professional training and the ability to handle potential complications.
It is worth noting that a successful spinal surgery does not guarantee immediate full health recovery; it may require time for recovery and effort to regain functions and mobility. It may also necessitate ongoing medical follow-up and physical therapy sessions to achieve optimal results.
In summary, the success rate of spinal surgery is generally high, but it depends on various factors. It is crucial to consult a specialized surgeon and be physically and mentally prepared for the surgery before making the final decision.
How long does back surgery take?
When people face back problems that do not respond to traditional treatment, surgery may be the only available solution. A common question people have is: how long does back surgery take? Here is a list of factors that may affect the duration of the surgery:
Type of Surgery: Partial Removal of Spinal Disc: May take between 45 minutes and two hours. Complete Removal of Spinal Disc: May take between two and three hours. Spinal Fusion Surgery: May take between two and three hours. Spinal Replacement Surgery: May require between three and four hours.
Patient’s Condition: Overall Health: If the patient is in good health and does not have other health issues, they may recover faster, and the surgery may take less time. Age: Age can affect recovery time, as elderly patients typically need more time for complete recovery. Extent of Back Problem: The deterioration of the back condition may affect the duration of the surgery. Rebuilding a vertebra may take between two and three hours to achieve a good result.
Special Needs: Associated Problems: If there are health problems requiring special attention, it may affect the surgery time. Previous Surgery: If the person has had previous back surgeries, the procedure may take longer due to the complexities of the situation.
Although these figures provide average surgery durations, it is important to emphasize that each case is unique, and the duration of the surgery and recovery period may vary. Patients should consult their treating physician to learn more about the probable time that back surgery will take in their particular case.
What are the most dangerous vertebrae in the spine?
The spine is considered one of the vital parts of the human body, as it supports the body and aids in movement. However, there are some vertebrae in the spine that are considered more dangerous than others. These vertebrae suffer from health problems and complications that can cause severe pain and disability.
Firstly, the lower cervical vertebra or vertebra C7 is one of the most dangerous vertebrae because it forms the interface between the neck and the upper back. If this vertebra is injured, such as in a car accident or a fall from a height, it can lead to fractures in the spine and damage to the surrounding nerves. This type of injury can significantly affect body movement and may require surgical intervention to repair.
Secondly, the first thoracic vertebra or vertebra T1 is also considered dangerous. This vertebra is located in the upper back area and is connected to the ribs. If this vertebra is seriously injured, the person may suffer from spinal fractures, and the respiratory and nervous systems may be affected. This injury can cause serious physical and functional problems that require immediate treatment and surgical intervention.
Thirdly, the fourth thoracic vertebra or vertebra T4 is also considered dangerous. This vertebra is located in the middle back area and is connected to the upper parts of the body such as the chest and lungs. Injury to this vertebra can cause chronic problems in breathing and movement. This injury may require surgery and a long period of physical therapy to restore normal body functions.
In addition, the fourth lumbar vertebrae require special care because they are in the area opposite the heart and lungs and can cause chronic problems in breathing and movement. People with other respiratory conditions, such as asthma or shortness of breath, should be particularly careful and take great care to avoid future problems.
In conclusion, there are many other vertebrae in the spine that could be dangerous if injured. However, the vertebrae mentioned above are some of the primary examples of the most dangerous vertebrae. Therefore, it is essential to handle the necessary care to maintain the health of the spine and avoid any injury that significantly affects movement and quality of life.
Does an Orthopedic Doctor Treat the Spine?
The spine is considered one of the vital parts of the human body, as it plays a role in supporting the bones, tissues, and muscles that aid in movement and stability. The spine can be subject to various problems and injuries that may affect an individual’s health and life.
In case of pain or injury in the spine, one might consult an orthopedic doctor to evaluate and diagnose the condition correctly. The specialized orthopedic doctor is the professional who treats and deals with diseases and injuries affecting the skeletal system, including the spine.
Under the doctor’s guidance, numerous tests and examinations related to the spine may be conducted to accurately identify the issue and comprehensively evaluate the condition. This might include X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scans of the spine.
Based on the final diagnosis, the orthopedic doctor will develop an appropriate treatment plan to address the spinal issue. This could include recommendations for rest and self-care, instructions for therapeutic exercises and strengthening the muscles surrounding the spine, and prescribing medications to relieve pain and inflammation.
In more complex and serious cases, and when there is a need for surgical intervention, the orthopedic doctor may refer the patient to a specialized spine surgeon. The spine surgeon uses advanced surgical techniques and precise tools to treat physical problems in the spine.
In summary, specialists in orthopedic medicine deal with diagnosing and treating various problems and injuries affecting the spine. If there is an issue with the spine, it is advisable to consult a specialized orthopedic doctor to get the correct diagnosis and appropriate treatment to help restore the spine to its proper state and improve quality of life.
When is Surgical Intervention Required for a Herniated Disc?
A herniated disc is a common issue that many people may experience. In many cases, symptoms can be improved and pain relieved through conservative treatments such as painkillers and physical therapy. However, some patients may require surgical intervention to address the herniated disc.
The factors considered for deciding to perform surgery to treat a herniated disc vary from one case to another. Here are some situations that might necessitate surgical intervention:
- Lack of Improvement After Conservative Treatment: If the patient continues to suffer from persistent pain, muscle spasms, and weakness in the lower extremities, and there is no improvement after a sufficient period of conservative treatment, then surgery might be the appropriate choice to alleviate symptoms and enhance quality of life.
- Severe Symptoms Occurrence: In some cases, a herniated disc can lead to direct pressure on the nerves and spinal cord, resulting in severe symptoms such as numbness, acute weakness in the legs, and loss of bladder control. If this condition is diagnosed, surgery may be the optimal choice to address the severe form of a herniated disc.
- Recurrent Herniated Disc: In some instances, the herniated disc may recur and continuously affect the quality of life. If symptoms regularly reappear despite following conservative treatments, then surgery might be an effective way to resolve the issue.
- Deterioration of Overall Health Condition: In certain cases, surgical intervention may be required when the herniated disc is the cause of a decline in the patient’s overall health condition. For example, there might be severe muscle weakness or a loss of ability to walk normally.
It is worth noting that the decision to undergo surgery is made based on the treating physician’s judgment, based on an evaluation of the patient’s individual condition and the symptoms they are experiencing. The patient should consult their treating physician to provide appropriate guidance and choose the best option for them.
Is Lumbar Spinal Fusion Surgery Dangerous?
Lumbar spinal fusion surgery is a surgical procedure used to treat various back problems, such as disc herniations, arthritis, and structural deformities. The lumbar vertebrae are stabilized using screws and metal plates, which helps improve the stability of the spine and reduce pain and muscle spasms.
Although this surgery is generally considered safe and effective, it does carry some risks and potential complications. The patient may experience temporary pain and swelling in the treated area after the surgery, but these symptoms usually disappear over time.
However, the patient should be aware of the rare complications that may include infection, bleeding, loss of nerve strength, and an allergy to the metals used in the stabilization. There is also a risk of persistent pain or deterioration of the condition after the surgery.
Therefore, the patient should discuss the risks and potential benefits of the surgery with the surgeon before making the final decision. The patient’s medical history should be reviewed, and necessary examinations should be conducted before the surgery to ensure that it is appropriate.
In general, if the surgery is performed by an experienced surgeon, and all health procedures and necessary precautions are followed, the chance of serious complications is very rare. However, the patient must be patient and strictly follow the surgeon’s instructions to achieve the best results and minimize potential risks.
When Can You Sit After Lumbar Spinal Fusion Surgery?
When a person experiences back or neck problems that require surgical intervention, clamps or plates may be installed to stabilize the affected or problematic vertebrae. After lumbar spinal fusion surgery, the patient often wonders how long they should wait before they can sit normally. In this section, we will review some important information on this topic.
The specific time to sit after lumbar spinal fusion surgery depends on several factors, such as the type of surgery performed and the complexity of the procedure. It is preferable to consult the treating surgeon about the required recovery period and return to normal sitting.
Generally, the patient should continue to lie flat on their back for a period of time after lumbar spinal fusion surgery. This is aimed at giving the resulting wound a chance to heal and recover.
The vertebrae may be stabilized to prevent them from moving or to correct a structural problem in the back or neck. In both cases, the required recovery period may vary.
After a rest period that typically lasts for several weeks, the patient gradually begins to move according to the surgeon’s instructions. Special physical therapy exercises may be used to enhance the recovery of strength and flexibility in the stabilized area.
The patient should follow the surgeon’s advice regarding lifting heavy weights and regular movement to avoid new injuries or movement of the stabilized vertebrae.
The goal of spinal fusion is to improve the function of the spine, reduce pain, and enhance movement. However, this procedure may require time for recovery and return to normal activity. The patient should adhere to the surgeon’s instructions and perform the recommended physical therapy to ensure the best results.
What are the Supports of the Spinal Column?
Spinal column supports are the structural elements that support and protect the spinal column, which is a vital part consisting of a series of vertebrae connected to each other. Supports are an indispensable part of the spinal column’s structure, maintaining its alignment, supporting, and reducing the load that this crucial part of the body bears.
There are several types of spinal column supports, including:
- Fibrous Bands: These are a type of connective tissue found around the vertebrae. Fibrous bands contribute to strengthening the spinal column and protecting it from injuries and pain.
- Back Muscles: The back muscles play an essential role in supporting and stabilizing the spinal column. These muscles extend along the spinal column, working to stabilize, move, and reduce pressure on it during movement.
- Intervertebral Discs: These are cartilaginous cushions found between the vertebrae, acting as shock absorbers to absorb pressure and impacts that the spinal column may experience. Intervertebral discs help to reduce friction between the vertebrae and contribute to the movement of the spinal column.
- Ligamentum Flavum: This ligament connects the vertebrae to each other and significantly contributes to the alignment of the spinal column. Ligamentum Flavum also helps to evenly distribute pressure across the connected vertebrae.
In summary, the supports of the spinal column are key factors that ensure the alignment and protection of the spinal column. They rely on fibrous bands, back muscles, intervertebral discs, and the ligamentum flavum, all working together to support and strengthen this vital part of the human body. A proper balance between these elements plays a significant role in the health and safety of the spinal column.
What are the Risks of a Disc Herniation Surgery?
The risks associated with disc herniation surgery are among the most significant health issues that people may encounter during their lifetime. It affects the spinal column, causing severe pain and reduced mobility. The potential causes of disc herniation are diverse, and undergoing surgery carries various risks. Here are some common risks that people should be aware of before deciding to undergo this procedure:
Anesthesia Risks: Disc herniation surgery requires general anesthesia, which carries its own specific risks. The medical team must assess the associated risks of anesthesia and ensure the patient’s safety during the procedure.
Infection Risk: The surgeon and their team must be extremely cautious regarding surgical safety and sterility for the patient. All necessary precautions must be taken to prevent contamination at the surgical site and maintain wound cleanliness.
Bleeding Risks: During the surgery, bleeding can occur at and around the surgical site. Surgeons need to optimize their techniques for controlling blood vessels and manage bleeding efficiently.
Wound Infection Risks: An infection can occur at the wound site post-surgery, which is a serious concern. Good surgical protocols must be applied to maintain wound cleanliness and minimize the risk of infection.
Risk of Surgery Failure: There is a possibility that the surgery might fail or that problems may persist after the procedure. The patient must understand this and be prepared for additional interventions post-surgery if necessary.