- Epidural Injections: In cases of severe lower back disc herniation, a doctor may recommend epidural injections. These injections are a medical procedure aimed at reducing pain and improving the condition of the herniated disc.
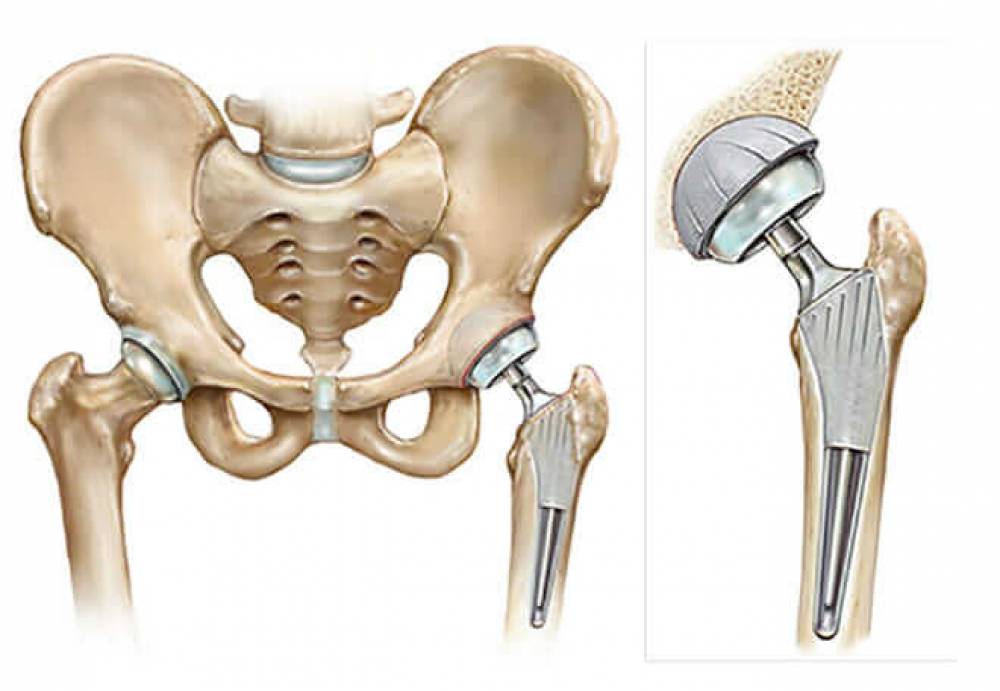
- Surgical Treatment: In cases with limited response to other treatments or in severe cases of lower back disc herniation, surgical treatment may be necessary. Surgical procedures for treating lower back disc herniation may involve removing the affected portion of the disc or performing a procedure to stabilize the spine.
Patients should take great care of their back health and safety and work on preventing back problems by engaging in regular exercise, avoiding heavy lifting, and maintaining proper sitting posture. Additionally, patients with lower back disc herniation should consult with specialized doctors to evaluate their condition and determine the appropriate treatment plan for their specific case.
What Is the Treatment for Lumbar Disc Herniation?
Lumbar disc herniation is a common problem that affects the lower back area, causing severe pain. It occurs when one of the discs between the vertebrae moves or slips out of place. The lower back region is most commonly affected by this issue, where patients experience intense pain.
There are several effective treatment options for lumbar disc herniation and relieving the associated pain. In this article, we will provide you with some effective ways to treat lumbar disc herniation:
- Use of Local Ice and Heat: Local ice and heat therapy are traditional and simple methods to relieve pain and reduce swelling. Placing an ice pack or a warm towel on the affected area for some time can help. Alternating between them or using one according to the patient’s preference can be effective.
- Pain-Relieving Medications: The treatment for lumbar disc herniation depends on the patient’s overall health and the severity of the pain. A wide range of medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), can be used to relieve pain and reduce swelling.
- Physical Therapy: Physical therapy can be employed to strengthen the back muscles and improve posture. Physical therapy includes stretching exercises, muscle strengthening exercises, and proper breathing techniques.
- Local Injections: In some cases, patients may be recommended to receive local injections in the affected area to relieve pain. These injections typically use corticosteroids or other local anesthetics.
- Surgery: Doctors may consider surgery in cases of lumbar disc herniation if symptoms do not improve with other treatments. The type of surgery required depends on the patient’s condition and the severity of the problem. Surgery may be performed using minimally invasive techniques to avoid complications.
Regardless of the chosen treatment, it is important to follow some guidelines to maintain the safety of the spine. Avoid heavy lifting and excessive bending of the back. Performing exercises that strengthen the muscles around the back can help promote spinal stability.
In conclusion, the appropriate treatment for lumbar disc herniation is one that aligns with the patient’s condition and specifically addresses the severity of pain and its overall impact on their daily life. Therefore, it is recommended to visit a doctor for an evaluation and to determine the suitable and individualized treatment plan.
What Are the Symptoms of Spondylitis?
Spondylitis is a health problem that some individuals may experience, and there are certain symptoms that may indicate the presence of this condition. Here is an article outlining the key symptoms of spondylitis and what you should know:
- Back Pain: Back pain is one of the common symptoms of spondylitis. The pain is often located in the lower back region and may extend to the hips and legs. People may describe the pain as continuous or intermittent, and it can worsen when sitting for extended periods or standing for prolonged periods.
- Difficulty in Movement: People with spondylitis may experience difficulty in movement. Bending the back or performing simple movements like lifting heavy objects or sitting for extended periods without pain may become challenging. Overall, movement may feel stiff and less flexible.
- Numbness or Tingling in the Legs: Some individuals with spondylitis may experience numbness in the legs or tingling sensations that spread from the lower back down to the feet. This numbness may be accompanied by a feeling of pins and needles or itching.
- Muscle Weakness: People with spondylitis may notice muscle weakness, especially in the leg area. They may have difficulty standing on their feet for extended periods or engaging in physical activities that require muscle strength.
- Swelling in the Affected Area: In cases of acute spondylitis, individuals may observe swelling in the lower back area. It is important to consult a doctor if the swelling persists for an extended period or is accompanied by severe pain.
Note: The symptoms of spondylitis can vary from person to person and depend on the characteristics of the condition and the severity of inflammation. Therefore, it is recommended to consult a doctor for an accurate diagnosis and to determine the appropriate treatment.
Please note that this information is for reference purposes only and does not replace consultation with a specialized doctor. Therefore, it is advisable to visit a doctor if you experience any of these symptoms, and if they persist for a long time or worsen over time.
What Causes Lower Back Pain Above the Buttocks?
Many people experience lower back pain that is accompanied by discomfort in the area of the back above the buttocks, and the cause may be related to several possible factors and reasons. In this article, we will explore eight common causes of back pain in this area.
- Muscle Spasms: Muscle spasms in the back are one of the primary causes of pain in the area of the back above the buttocks. Spasms can occur due to muscle tension or excessive stress and may result in pressure on surrounding nerves, leading to pain.
- Upper Lumbar Spine Pain: The upper lumbar spine contains a group of vertebrae, and issues in these vertebrae can cause back pain above the buttocks. These issues may be the result of muscle contractions or nerve compression in the surrounding area.
- Joint Friction: Friction in the joints located in the back above the buttocks can be a common problem causing pain. Joint friction may occur due to arthritis or damage to the cartilage.
- Herniated Disc: A herniated disc may be one of the reasons leading to pain in the back above the buttocks. Herniated discs happen when the discs between spinal vertebrae are damaged, resulting in pain and nerve compression.
- Sciatic Nerve Pain: Some individuals may experience back pain above the buttocks due to irritation of the sciatic nerve. This occurs when the nerve is compressed or injured, resulting in sharp pain that radiates from the back down to the legs.
- Ligament Strain: The ligaments in the back above the buttocks may stretch or tear, causing pain and a feeling of tension in the area. This can occur due to sudden movements or excessive spine stretching.
- Arthritis: Arthritis in the spinal column can lead to pain in the back above the buttocks. Arthritis occurs when the cartilage between joints is damaged, causing pain, swelling, and stiffness in the back.
- Spinal Misalignment: Spinal misalignment can be a cause of back pain above the buttocks. Misalignment occurs when the axis of the spine deviates from its correct position, resulting in pain and tension in the back.
Pain in the back above the buttocks is a common issue, and there are several possible causes for this type of pain. These causes may include muscle spasms, vertebral problems, joint friction, herniated discs, sciatic nerve pain, ligament strain, arthritis, and spinal misalignment. If the pain persists or worsens, it is advisable to consult a doctor for an evaluation and an accurate diagnosis of the underlying cause.
How Does a Herniated Disc Patient Sleep?
Herniated disc disease is a condition that affects many people around the world. One crucial aspect of improving patients’ conditions is getting good and proper sleep. Although pain and discomfort can be a hindrance during sleep, there are several ways to enhance sleep quality and alleviate symptoms associated with herniated discs. In this article, we will provide you with 10 proper ways to improve the sleep of a herniated disc patient.
- Use Supportive Pillows: Choosing appropriate pillows with good support helps reduce pressure on the spine and minimizes pain. It is recommended to use curved pillows to support the neck correctly.
- Sleep on Your Back with a Supportive Pillow: It is advised to sleep on your back with a pillow under your head and another pillow under your knees. This position helps align the spine and reduce pressure on the spinal discs.
- Sleep on Your Side with a Leg Pillow: Patients can also sleep on their sides with a pillow placed between their legs. This position helps stabilize the spine and reduces spinal disc friction.
- Avoid Sleeping on Your Stomach: Sleeping on the stomach should be avoided as it can lead to excessive strain on the spine, increased pain, and pressure on the spinal discs.
- Choose a Suitable Mattress: Ensure that you select a mattress that provides the necessary support for the spine. It is preferred to use a medium-firm mattress for the best comfort.
- Relax Before Bed: Practice relaxation techniques before bedtime, such as deep breathing and muscle relaxation exercises, to reduce tension and calm the body and mind.
- Avoid Sudden Movements in Bed: Try to avoid sudden movements and turning in bed, as these movements can increase pain and irritate the nerves.
- Use Heat Therapy: Heat therapy methods such as heating pads or heated belts can be used to help alleviate pain and muscle tension before sleep.
- Engage in Moderate Exercise: Regularly engage in moderate exercises to strengthen the back and abdominal muscles and improve spinal alignment.
- Consult a Doctor: If symptoms persist, and sleep quality deteriorates, it is advisable to consult a specialist doctor to evaluate the condition and provide appropriate advice and treatment.
It is essential to focus on sleep quality for herniated disc patients to improve their condition and reduce the pain they experience. The above methods can be applied to enhance sleep quality and achieve better comfort during sleep. In any case, it is recommended to consult with a specialist doctor before making any changes or starting new treatment programs.
Can Herniated Discs Heal?
Among the chronic conditions that affect a large number of people worldwide, herniated discs are at the forefront of these conditions. Herniated discs are a common problem that affects the spinal discs and can, in severe cases, lead to chronic pain and numbness in the lower limbs.
Despite the prevalence of this condition, many patients wonder if there is hope for a complete recovery from herniated discs. In this article, we will provide you with a comprehensive answer to this question, based on current studies and medical experiences.
- Early Diagnosis and Immediate Treatment: Early diagnosis and starting treatment may contribute to better outcomes.
- Physical Therapy and Back Muscle Strengthening: Physical therapy, improving strength, and flexibility are essential aspects of treatment.
- Medication: Pain-relieving and non-steroidal anti-inflammatory medications such as acetaminophen and ibuprofen can be options to alleviate pain and associated inflammation.
- Self-Care Measures: Patients should follow appropriate self-care measures, including rest, avoiding excessive strain, and avoiding excessive bending of the back. It is also essential to maintain proper sitting and sleeping postures to reduce spinal disk pressure.
- Non-Surgical Approaches: In some cases, non-surgical techniques can be applied to treat herniated discs, such as massage, physical therapy, and therapeutic injections. These techniques can help reduce pain and improve overall back movement and function.
- Surgery: Responding to non-surgical treatments is the optimal choice for many patients. However, in severe cases where non-surgical treatments are ineffective, doctors may recommend surgery.
Surgery is considered the last resort and is only performed in specific cases.
With regular consultation with specialized doctors and following the necessary treatment steps, patients can overcome herniated disc pain and regain normal abilities to perform daily activities. However, it’s important to note that each case may yield different results, and treatment guidance and recommendations should be tailored to individual conditions and severity. By consulting with a specialist doctor and working with a healthcare team, patients can lead a normal life and potentially achieve a partial or complete recovery from herniated discs, depending on their personal circumstances.