“What is the treatment for hidradenitis suppurativa, and learn about possible risks.”
أخر تحديث :
Treatment of Hidradenitis Suppurativa
Hidradenitis suppurativa is a painful condition that causes inflammation and pain in the muscles and tendons that run along the side of the leg. This problem is common among people who engage in intense sports or strenuous activities. Fortunately, there are several methods that can be used to treat hidradenitis suppurativa, alleviate pain, and improve mobility. In this article, we will outline the top 10 ways to treat hidradenitis suppurativa.
- Use of Anti-Inflammatory Drugs: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen are among the most effective medications for treating hidradenitis suppurativa. These drugs work to reduce pain, swelling, and muscle movement.
- Corticosteroids: In severe cases of hidradenitis suppurativa, a doctor may prescribe topical corticosteroids containing cortisone. These medications help reduce swelling and inflammation in the affected area.
- Antidepressant Medications: Antidepressant medications may be prescribed by a doctor if hidradenitis suppurativa is accompanied by psychological stress or mood disorders. These drugs work to improve mood and reduce pain associated with the condition.
- Muscle Relaxants: In some cases, a doctor may prescribe muscle relaxants to alleviate spasms and muscle knots that may worsen the symptoms of hidradenitis suppurativa.
- Over-the-Counter Pain Relievers: Over-the-counter pain relievers such as acetaminophen, ibuprofen, and naproxen can be used to alleviate pain associated with hidradenitis suppurativa. However, it is important to consult a doctor before using them for extended periods.
- Home Treatment and Exercises: A doctor may recommend home treatments, including applying ice or heat to the affected area, as well as performing appropriate exercises to strengthen and stretch the affected muscles.
- Massage Therapy for Hidradenitis Suppurativa: Massage therapy is considered a complementary treatment for hidradenitis suppurativa. It helps improve blood circulation, reduce tension, and relax tense muscles.
- Cupping Therapy: Some people recommend cupping therapy sessions to treat hidradenitis suppurativa. Cupping therapy increases blood flow to the affected area and improves blood circulation.
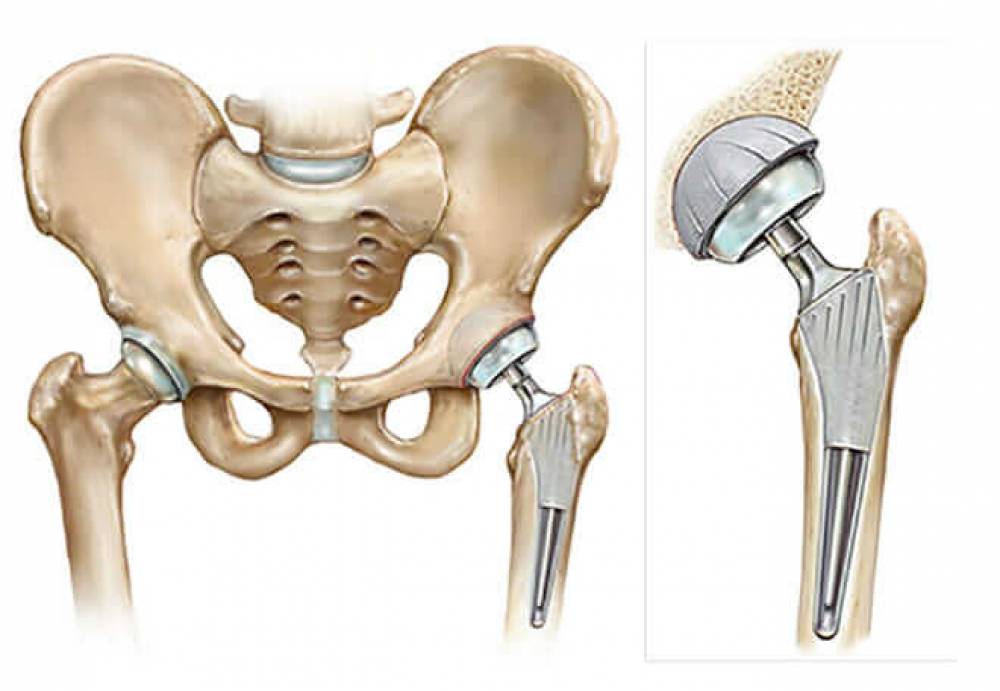
- Surgery: In extremely rare cases where chronic hidradenitis suppurativa does not respond to any non-surgical treatments, surgical intervention may be the option. In such cases, the narrow passage is opened, and pressure on the affected nerve is relieved.
- Self-Care and Prevention: One of the most important things you can do to prevent hidradenitis suppurativa is to avoid excessive exertion and warm-up and stretch your muscles before engaging in any physical activity. Additionally, it is advisable to wear appropriate shoes and use protective measures such as insoles and cushions to strengthen the muscles and maintain overall leg health.
Hidradenitis suppurativa can be extremely painful and can impact a person’s life. However, with proper treatment and self-care, the condition can improve, and symptoms can fade over time. If you are suffering from hidradenitis suppurativa, we recommend consulting a specialist doctor to assess your condition and develop an appropriate treatment plan.
Natural Treatment for Sciatica
Sciatica, also known as “sciatic nerve inflammation,” can cause severe pain and restrict body movement. Despite the availability of conventional treatment options, which include pain medications, physical therapy, and surgery, many people prefer to use natural remedies to alleviate symptoms and promote healing.
In this article, we will take a look at 10 effective natural methods for treating sciatica:
- Hot or Cold Compresses: Applying hot or cold compresses is considered one of the most effective ways to relieve sciatica pain and inflammation. Thermal therapy helps relax tense muscles that may compress the sciatic nerve. Using moist compresses, such as a steam towel, is preferred for maximum benefit.
- Therapeutic Massage: Therapeutic massage is considered a useful method for reducing tension, muscle spasms, and improving blood flow. Massage can reduce sciatica pain and enhance the body’s ability to recover.
- Exercise: Engaging in appropriate exercises can help alleviate sciatica pain and increase muscle flexibility. This may require guidance from a physical therapy specialist to ensure that exercises are safe and effective.
- Pillow Support: Placing a pillow under the hip or the painful area can provide support and relieve pressure. This can help reduce sciatica pain and increase comfort while sitting or lying down.
- Traction or Stretching Tools: The use of traction or stretching tools can assist in lengthening the spine and relieving pressure on the sciatic nerve. These tools should be used under the supervision of a specialist as part of a specific treatment program.
- Dietary Supplements: Some dietary supplements, such as vitamin B12, calcium, and magnesium, may help strengthen muscles and alleviate sciatica pain. Consultation with a doctor is necessary before taking any dietary supplements to ensure the appropriate dosage and safe usage.
- Herbal Remedies: Some herbal remedies are used to treat sciatica and reduce pain, such as ginger, turmeric, and aloe vera. These herbs can be used in the form of natural supplements or consumed in foods and beverages.
- Stress Management: Avoiding excessive stress and tension is essential as they can negatively impact sciatica and increase pain. Deep breathing techniques, relaxation, and meditation can help control stress and alleviate symptoms.
- Physical Rehabilitation: Medical rehabilitation is an essential part of treating sciatica, helping improve mobility and strengthen affected muscles. Physical rehabilitation may include muscle strength exercises, stretching, and balance improvement exercises.
- Acupuncture: Acupuncture is often used in alternative medicine to treat sciatica. It is believed to stimulate the immune system and promote the body’s natural healing process. This treatment should be performed by a qualified and certified specialist.
Sciatica can be a painful and bothersome condition, but there are many natural methods that can be used to alleviate symptoms and expedite the healing process. By using hot or cold compresses, therapeutic massage, engaging in appropriate exercises, and implementing other natural remedies, individuals can reduce sciatica pain and regain their mobility effectively. However, people should consult with a qualified healthcare specialist regarding appropriate preventive and treatment measures.
What Causes Sciatica and How Is It Treated?
Sciatica, also known as sciatic nerve inflammation, is a common medical condition that causes back and lower extremity pain. This pain occurs due to irritation and inflammation of the sciatic nerve, which runs from the lower part of the spinal cord down the back to the leg and foot.
Sciatica typically occurs as a result of sudden pressure or irritation on the nerve below the spinal column. This pressure can be caused by a herniated disc, a condition in which the gel-like fluid inside the discs between the vertebrae protrudes, compressing the surrounding nerves and causing pain in the lower back that may extend down the leg.
One of the main differences between sciatica and a herniated disc is the duration of treatment required for each condition. Sciatica can typically be treated over a shorter period, while treatment for a herniated disc often requires a longer duration and is frequently a chronic problem.
Symptoms of sciatica include sharp pain in the lower back and buttocks, a sensation of numbness and tingling in the lower extremities, and muscle weakness. Pain may worsen when sitting for extended periods, with sudden movements, or when lifting heavy objects.
Several treatment options are available for sciatica, depending on the severity of symptoms and their impact on the patient’s quality of life. Patients are often advised to make lifestyle changes and adopt daily habits to alleviate symptoms. Some of these changes include:
- Rest and maintaining a comfortable posture: It is advisable to avoid sitting or standing for long periods and to ensure proper body posture when sitting and sleeping.
- Exercise and stretching: There are exercises that help strengthen the muscles surrounding the sciatic nerve and reduce pressure on it. Patients may be advised to visit a fitness trainer or physical therapist to receive appropriate exercises.
- Medication: Medications are commonly used to reduce pain and swelling. These include non-steroidal anti-inflammatory drugs (NSAIDs) and pain-relief medications.
- Physical therapy: This may include massage, heat therapy, and spinal adjustments. Physical therapy can help reduce pain and improve range of motion.
- Interventional treatments: In severe cases where symptoms do not respond to other treatments, interventions such as localized injections or surgery may be suggested.
Over time, most individuals with sciatica experience improvement in their condition, with a gradual reduction in the severity of symptoms. However, some cases may continue to experience pain or develop other complications. Therefore, it is recommended to consult a doctor to diagnose the patient’s condition and determine the best treatment plan.
Sciatica is a common condition that affects thousands of people. By consulting with a healthcare professional and following their advice, it is possible to overcome symptoms and achieve a better quality of life. Do not hesitate to ask any questions related to sciatica to specialized doctors for advice and appropriate treatment.
What Causes Sciatica in the Right Leg?
Sciatica in the right leg is a condition where an individual experiences pain that radiates from the lower back, wraps around the hips and buttocks, and extends down the leg. Sciatica is a type of back pain caused by pressure on the sciatic nerve. It can lead to feelings of nausea, leg weakness, and muscle tension.
What are the causes of sciatica in the right leg?
The symptoms of sciatica in the right leg occur when there is irritation at the root of the sciatic nerve or constriction in the lumbar spinal canal. Irritation of the sciatic nerve can result in severe symptoms of sciatica. Additionally, lumbar spinal canal constriction can compress the sciatic nerve and lead to the development of sciatica symptoms.
Furthermore, there are other common causes of sciatica in the right leg, including:
Lumbar spinal stenosis: Narrowing of the spinal canal in the lower back, which can compress the sciatic nerve.
Herniated disc: The protrusion of spinal discs in the vertebral column, which can cause pressure on the sciatic nerve and the appearance of sciatica symptoms.
Facet joint inflammation: Inflammation of the facet joints in the spinal column area can irritate the sciatic nerve and lead to the development of sciatica.
Piriformis syndrome: If the piriformis muscle in the buttocks compresses the sciatic nerve, it can result in sciatica symptoms.
Trauma or accidents: Sciatica in the right leg may occur due to injuries or accidents that cause pressure on the sciatic nerve.
What are the common symptoms of sciatica in the right leg?
The severity and quality of symptoms experienced by individuals with sciatica in the right leg may vary. However, there are some common symptoms that may indicate the presence of this condition, including:
Pain in the lower back, buttocks, and down the leg, which can range from mild to severe.
Feelings of numbness or tingling in the leg or foot.
Muscle weakness in the leg or foot.
Difficulty in movement and walking.
Muscle tension or spasms in the leg or foot.
A sensation of pins and needles or burning in the leg or foot.
What Are the Potential Complications of Sciatica in the Right Leg?
In most cases, sciatica in the right leg typically recovers without treatment within a few weeks. However, some cases may lead to serious complications. Potential complications of sciatica in the right leg include:
Permanent nerve damage: Chronic pressure on the sciatic nerve may result in permanent nerve damage, leading to lasting changes in sensation and movement.
Pelvic control issues: Sciatica can lead to weakness in the pelvic muscles, causing difficulty in controlling urination or experiencing involuntary urination.
Muscle weakness: Sciatica may cause weakness in the leg or foot muscles, affecting the ability to walk and perform daily activities.
How to Prevent Sciatica in the Right Leg?
While it may not always be possible to prevent sciatica, there are some measures that can be taken to reduce the risk of its occurrence, including:
Regular exercise to strengthen the muscles of the back, buttocks, and legs.
Maintaining a healthy weight and avoiding excessive weight gain.
Relaxation techniques to reduce stress and pressure on the sciatic nerve.
Avoiding improper lifting techniques when handling heavy objects and using proper weightlifting techniques.
Avoiding prolonged periods of standing or sitting without movement and minimizing exposure to excessive vibrations or shocks on the back.
Using comfortable pillows for sleep and a suitable mattress for back support.
When Should You Visit a Doctor?
In the case of sciatica in the right leg, most individuals respond to non-surgical treatments within a few weeks and fully recover. However, it may be necessary to visit a doctor if the symptoms persist for an extended period or if the symptoms worsen significantly.
How I Recovered from Sciatica: 10 Effective Methods
Sciatica is a common medical condition that causes severe pain in the sciatic nerve, and it is a common issue. If you are suffering from sciatica and looking for effective ways to alleviate it, you may find these reliable and tried methods helpful. Here are the top 10 ways to treat sciatica:
Pain relieving medications: Over-the-counter pain relievers like acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can help alleviate the pain associated with sciatica. However, it is advisable to consult a doctor before using them for extended periods.
Physical therapy: Physical therapy can help strengthen the muscles surrounding the affected nerve, improve mobility, and reduce pain. It includes stretching exercises, muscle strengthening, and core stability exercises.
Heat therapy: Applying heat to the affected area can help alleviate pain and soothe the irritated nerve. Methods such as heating pads or warm, moist towels can be used.
Massage: Massage can help relieve tension and muscle spasms, increase blood flow to the affected area, and reduce pain. It’s important to perform massage gently and with proper technique to avoid further irritation of the nerve.
Electrotherapy: Electrotherapy is used to stimulate muscles and relieve pain by directing electrical currents to the affected area. This therapy should be administered under the supervision and guidance of a rehabilitation specialist.
Nerve injections: Nerve injections involve directly injecting medications into the affected area to relieve pain and calm the irritated nerve. This procedure is performed under the supervision of a doctor and may require multiple sessions.
Acupuncture: Traditional acupuncture can be used to stimulate specific points in the body to improve energy flow and reduce pain. This therapy is based on principles of traditional Chinese medicine.
Surgery: Surgery may be necessary in severe cases of sciatica that cause significant leg weakness or involve bowel or bladder changes. Surgical procedures include decompressing the nerve or removing excess bone structures.
Breathing and relaxation training: Breathing and relaxation techniques can help reduce stress and pain associated with sciatica. These techniques can be learned through consultation with a specialist.
Lifestyle changes: Making changes to your lifestyle can be beneficial in reducing sciatica symptoms. This includes avoiding unhealthy habits like smoking, maintaining a healthy diet, and increasing physical activity levels.
There is no one-size-fits-all treatment, and each individual may need to try multiple methods to alleviate sciatica symptoms. It’s important to consult with a doctor to determine the best treatment plan that suits your personal condition.
Does Sciatica Show Up on X-Rays?
Sciatica is a medical condition characterized by pain and numbness in the hip, thighs, and legs. Some may wonder if X-rays can reveal the presence of this condition. In this article, we will explore the possibility of detecting sciatica on X-rays and methods of diagnosis.
Using X-Rays for Diagnosing Sciatica: Your healthcare provider may request certain imaging tests to determine your diagnosis. Among these tests, X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) can be used to detect any structural changes in the spine or hip area.
Physical Examination for Sciatica: During a physical examination, the doctor will assess the strength of your muscles and your response. You may be asked to lift your legs or move your toes for testing. If these movements cause pain and numbness in the affected area, it may indicate the presence of sciatica.
Accompanying Symptoms of Sciatica: It’s worth noting that sciatica usually occurs on one side of the body only. The pain can be sharp and debilitating, causing numbness and weakness in the affected leg. You may also feel pain in the hip or the back of the thigh.
Treatment for Sciatica: In most cases, sciatica symptoms can be relieved using non-surgical measures after a few weeks. Non-surgical treatment includes pain relief with analgesics, improving sitting and sleeping positions, and following exercises to strengthen the back and hip muscles. Your doctor may recommend physical therapy sessions or the use of transcutaneous electrical nerve stimulation (TENS) to alleviate pain.
Surgery as a Treatment for Sciatica: Surgery is typically performed in cases of severe sciatica, where the pain becomes unbearable. Surgery may also be required when a patient cannot control bowel or bladder function, or if symptoms do not improve with other treatments.
Therefore, X-rays can reveal the presence of sciatica by detecting changes in the structure of the spine or hip area. However, an accurate diagnosis of sciatica requires consultation with your specialized healthcare provider and a physical examination. Always remember that appropriate treatment necessitates a proper diagnosis and ongoing monitoring by a specialized medical team.
What Is the Difference Between Sciatica and a Herniated Disc?
Both men and women face various health issues related to sciatica and herniated discs, but there are differences in symptoms and treatment. Here is a list of key differences between sciatica and a herniated disc to help you better understand these two conditions.
Definition of Hot Flashes:
Hot flashes refer to sudden waves of internal heat in a woman’s body, often accompanied by flushing or reddening of the face, neck, and chest. Other symptoms that may accompany hot flashes include increased heart rate, muscle tension, and nausea. Hot flashes can occur due to hormonal changes that occur during perimenopause and postmenopause.
Definition of Herniated Disc:
A herniated disc, or herniated vertebral disc, is a medical condition associated with damage to the disc in the spinal column. It is characterized by pain in the back, which can radiate to the lower limbs. A herniated disc can occur due to repetitive pressure on the spinal column or joint inflammation.
Differences in Symptoms:
Hot flashes and herniated discs differ in their accompanying symptoms. When hot flashes occur, a person feels a sudden sensation of heat and redness in specific areas of the body. In the case of a herniated disc, it causes sharp pain in the back, which can extend to the lower limbs.
Differences in Treatment:
The treatment of hot flashes and herniated discs varies significantly. Although hot flashes can be uncomfortable and tiring, they are considered a natural and non-serious phenomenon. Women can manage hot flashes by reducing the consumption of stimulating substances such as caffeine and taking simple measures like wearing appropriate clothing and creating a comfortable environment for rest. As for a herniated disc, treatment usually involves conservative measures such as lifestyle changes and exercises to strengthen the muscles around the spinal column. In more severe cases, surgery may be required.
Consulting a Doctor:
If you are experiencing severe symptoms of hot flashes or a herniated disc, it is advisable to consult your doctor for an accurate diagnosis and appropriate treatment. Your doctor may request additional tests such as X-rays or magnetic resonance imaging (MRI) to better evaluate your condition.
Hot flashes and herniated discs are two different medical conditions with varying symptoms and treatment approaches. Hot flashes can be a temporary nuisance, while a herniated disc is a significant health condition that requires substantial care. Therefore, consulting with your doctor when experiencing any of these symptoms is recommended.
Does Walking Affect Hot Flashes?
Hot flashes can be a painful condition that many people suffer from, leading to limitations in their daily activities and prolonged periods of sitting. Exercise, including walking, is one of the best ways to alleviate the pain of hot flashes and improve overall quality of life. Among these beneficial activities, walking tops the list of sports that can help alleviate the pain of hot flashes.
A study conducted on 35,000 individuals found that walking or cycling led to a 33% reduction in the risk of experiencing hot flashes. Therefore, the answer to the question of whether walking is beneficial for someone with hot flashes is often positive.
But how can you maximize the benefits of walking in relieving hot flashes? That’s what we’ll discuss in this article.
- Regular Walking Practice: To achieve the best results, it is recommended to engage in walking regularly. Set aside daily time for walking and try to maintain this healthy habit. You may start with short sessions initially and gradually increase the duration of your walks until you reach 30-45 minutes per session.
- Choosing Suitable Terrain: When selecting the path for your walk, try to choose soft and non-hard terrain as much as possible. Make walking a part of your daily routine and include it in a location close to your home or workplace. Maintaining Good Posture: During your walk, ensure that you maintain good posture. Walk with natural steps, relax your muscles, and avoid tension while walking.
- Stretching and Muscle Strengthening Exercises: Before starting your walk, perform stretching exercises to warm up your muscles and increase their flexibility. After finishing your walk, do exercises to strengthen the muscles of your back and core to improve stability and reduce nerve pain.
- Consulting a Doctor: Before continuing with walking or any other type of physical exercise, it is important to consult your doctor. They can provide additional advice and specific guidance based on your health condition and the severity of your pain.
Walking is considered an ideal sport for people suffering from hot flashes and can contribute to improving their quality of life. However, walking should be done correctly and in moderation. Consult your doctor and take care of your health while engaging in this activity.
What Are the Risks of Hot Flashes?
Hot flashes are a painful condition that affects specific parts of the human body, presenting a health challenge for many individuals. The phenomenon of hot flashes can be very exhausting and causes a lot of concern due to the persistence of severe pain and its widespread occurrence throughout the body. In this article, we will discuss a range of factors associated with hot flashes that individuals should take into consideration for prevention and management.
- Age: Age is considered a significant factor in the occurrence of hot flashes. According to studies, the risk of developing this condition increases as a person gets older. This may be due to changes that occur in the body with advancing age, such as disc herniation and bone degeneration.
- Physical Strain: Strenuous physical activities and heavy weightlifting are considered risk factors associated with hot flashes. When the spine is subjected to excessive pressure or tension, it can lead to hot flashes. Therefore, individuals should avoid heavy lifting and take preventive measures during physical activities.
- Obesity: Unfortunately, obesity is a risk factor associated with hot flashes. Excess weight leads to increased pressure on the spine and adjacent nerves, increasing the likelihood of hot flash symptoms. Therefore, individuals who are obese should work on weight loss and overall physical fitness improvement.
- Medical Conditions: There are certain medical conditions that increase the risk of a person developing hot flashes. This includes spinal infections, diabetes, nerve tumors, and pelvic inflammations. Therefore, seeking medical advice and properly treating these conditions can reduce the likelihood of hot flash symptoms.
- Smoking: It is known that smoking has a negative impact on overall health. Concerning hot flashes, smoking reduces the body’s ability to repair and regenerate tissues, including spinal tissues, which increases the risk of hot flashes. Therefore, smokers should quit this harmful habit.
- Genetics: Genetic factors may play a role in increasing the likelihood of hot flashes. If family members have a history of spinal problems, there may be a greater likelihood of hot flashes occurring. In this case, individuals should consult their doctor and take appropriate preventive measures.
Individuals should take these factors associated with hot flashes into consideration and adopt a healthy lifestyle while regularly engaging in physical exercise. They should also follow medical guidance and safety precautions related to preventing this painful condition.