What are the symptoms of a disc in the back? And how should a patient with a disc herniation sleep? What are the symptoms of a disc in the back?
أخر تحديث :
What are the symptoms of a disc in the back?
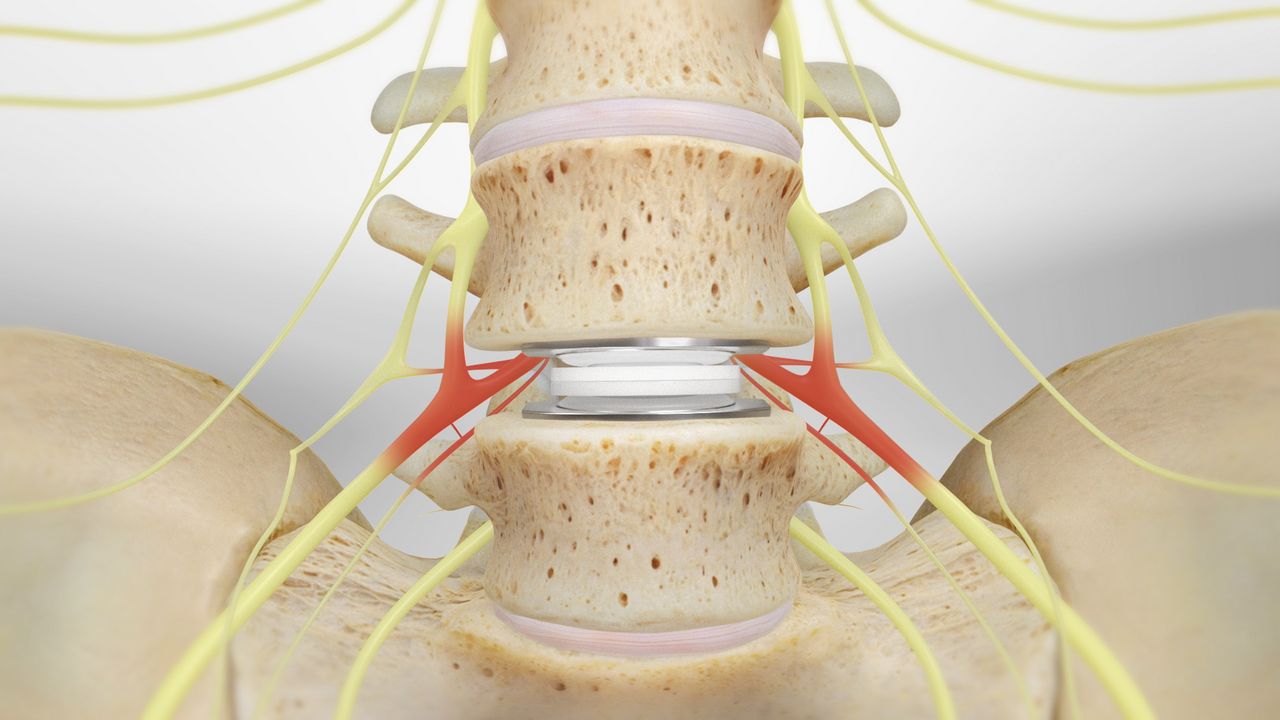
A herniated disc in the back is a condition that occurs when the disc between the vertebrae in the spine moves out of its normal position. A herniated disc can cause painful symptoms and affect the movement of the affected person. Here are some common symptoms of a herniated disc in the back:
- Persistent lower back pain: The affected person may experience constant pain in the lower back area. The pain can be sharp and persistent or intermittent and vary in intensity.
- Stiffness in the legs or lower back: The affected person may feel stiffness in the leg muscles or lower back area. This can affect their ability to move freely and normally.
- Pain when pressing on the lower back area: The affected person may feel pain when pressing on the lower back area or performing certain movements such as bending or sitting for long periods.
- Pain in the thigh: The affected person may feel pain that extends from the back to the thigh. The pain can be sharp and persistent or may only be felt during certain specific movements.
- Difficulty walking or standing for long periods: The affected person may find it difficult to walk for long periods or stand for extended periods due to pain and stiffness in the back and legs.
- Pain when bending: The affected person may experience sharp pain when bending or trying to perform movements like heavy lifting or bending forward.
- Feeling of pins or numbness in the feet: The affected person may experience pins or numbness in the feet due to the disc pressing on the nerves in the spine.
The causes of a herniated disc in the back can vary and include factors such as aging, excessive stress on the spine, sports injuries, and structural abnormalities in the spine. Genetic factors may also play a role in increasing the likelihood of a herniated disc.
To prevent a herniated disc in the back, some preventive measures can be followed, such as:
Maintaining good body posture while sitting, standing, and lifting heavy objects. Performing exercises that strengthen the muscles of the back, abdomen, and legs. Avoiding strong movements and spinal twists. Maintaining a healthy weight and eating a balanced diet. Avoid sitting for long periods without movement and doing stretching and strengthening exercises for the muscles.
In conclusion, if you suffer from any of the above symptoms, it is essential to seek medical advice and undergo the necessary examinations to diagnose your condition and determine the appropriate treatment.
What is the best treatment for back disc problems?
A back disc or herniated disc is a condition where a disc between the vertebrae near the spine slips out of place. A herniated disc can cause severe pain and muscle spasms in the back area. Therefore, many people seek the best ways to treat back disc problems.
There are several effective methods to treat a herniated disc in the back without the need for surgery. Among these methods are lifestyle changes, resorting to physical therapy, and using pain relief medications. Here are some traditional methods used in treating herniated discs in the lumbar vertebrae:
Resting in bed for good periods interspersed with standing or walking for short times; to avoid stiff muscles and joints. Using cold or hot compresses on the area of pain to relieve pain and swelling. Practicing stretching exercises to maintain muscle flexibility and strengthen the vertebrae and discs. Resorting to physical therapy, where the physiotherapist guides the patient to perform specific exercises to strengthen the muscles and improve flexibility. Avoiding standing for long periods and sitting in the correct posture, and if there is a need to stand for a long time, placing one of the feet on a small box to reduce pressure on the back. Reducing weight, as excess weight leads to an increased load on the spine. Quitting smoking, as smoking can cause arterial stiffness and damage to the cartilage.
Treatment of herniated disc in the back also depends on the general health of the patient and the severity of the pain. The patient may resort to using painkillers and pain relief medications to reduce pain and muscle spasms in the back initially. If the pain continues and the condition worsens, surgical treatment may be necessary.
It is important to consult a specialist doctor before adopting any treatment methods for a herniated disc in the back. The doctor should evaluate the condition and determine the appropriate treatment based on the patient’s condition and medical history. The doctor may prescribe physiotherapy sessions or prescribe suitable pain relief medications to alleviate pain and improve the patient’s overall condition.
In summary, there are many effective methods available for treating a herniated disc in the back without the need for surgery. Among these methods are lifestyle changes, practicing suitable physical exercises, and using pain relief medications. It is advisable to see a specialist doctor to evaluate the condition and determine the appropriate treatment according to the patient’s condition.
How should a patient with a herniated disc sleep?
Patients with a herniated disc in the neck face significant challenges when trying to sleep properly. Pain and stiffness in the neck can affect the quality of sleep and cause discomfort and unease. Therefore, patients must follow specific recommendations for proper sleep and to maintain the health of the spine.
One of the recommended positions for patients with a herniated disc in the neck is to sleep on their back with a pillow under the knees. This position involves lying on the back with a pillow under the head and extending the feet forward with another pillow under the knees. This position helps to extend the neck muscles and relieve stiffness. This position should be maintained for a minute.
Another recommended sleeping position is to sleep on the stomach with a pillow underneath. This position requires laying the body on the stomach with a pillow under the head and facing the head to one side. A thin pillow should also be placed in the upper chest area and another pillow under the lower abdomen. This position helps to reduce pressure on the vertebrae.
Additionally, it is recommended to avoid sleeping on the stomach with the head turned to the side, as this can cause deformities in the spinal column and increase pain.
The bed or surface on which the patient sleeps should be comfortable and appropriate to maintain the spine’s alignment. Support pillows for the neck and back can be used to provide necessary support and reduce pressure on the vertebrae.
In addition to the recommended sleeping positions, patients with cervical disc herniation should avoid activities that increase pain and tension in the neck before sleeping, such as sitting for long periods or performing intense exercises. Ice or localized heat can also be used to relieve pain before sleeping.
Ultimately, patients with cervical disc herniation should consult their treating physician to obtain specific recommendations for their individual condition. The doctor can help assess the condition and determine appropriate positions and provide the necessary advice to improve sleep quality and relieve pain.
Is a herniated disc dangerous?
A herniated disc, or disc herniation, is a common condition that causes back pain. It occurs when part of the soft disc in the spine bulges out, causing pressure on the surrounding nerves, leading to pain and numbness in the back and legs. While a herniated disc can be painful and troublesome, it is usually not dangerous.
Disc herniation is a common condition and can happen to anyone at any age. Although the pain may sometimes be severe, most cases of disc herniation improve with conventional treatments such as physical therapy, exercise, and pain medications.
However, there are some rare cases where a herniated disc can be dangerous. For example, if there is severe pressure on the surrounding spinal nerves, muscle weakness or loss of sensation in the legs may occur. In other rare cases, surgery may be needed to remove the slipped part of the disc.
Early detection and appropriate treatment of a herniated disc are crucial. This may require visiting a spine doctor or rheumatologist for diagnosis and to determine the proper treatment. Treatment may include physical therapy, targeted exercises, and pain relief medications.
To prevent disc herniation, some simple tips can be followed. It’s important to maintain proper body posture while standing and sitting, and to avoid sitting for long periods without movement. One should also avoid lifting heavy weights incorrectly and make sure to use proper weight lifting techniques.
Generally, it can be said that disc herniation is not generally serious and can be successfully treated in most cases. However, individuals experiencing chronic or severe symptoms should visit a doctor to assess their condition and determine the appropriate treatment. Prevention and early treatment can help avoid complications and improve the quality of life.
How long does the pain from a disc herniation last?
A disc herniation is a condition that occurs when part of the disc that lies between the vertebrae of the spine slips out of place and can cause severe pain and muscle spasms. The duration of pain in the case of disc herniation depends on several factors, including the severity of the condition and the patient’s adherence to the prescribed treatment.
Recovery from disc herniation typically takes about 4-6 weeks. During this period, the prescribed treatment by a specialist doctor, which may include pain relievers or cortisone injections among others, is administered. After the recovery period, a gradual return to normal activity is recommended. It is important for the patient to achieve complete healing during this period by adhering to the treatment and following the specialist’s guidance.
However, it should be noted that the recovery duration from disc herniation is not fixed in all cases. This period may vary depending on the severity of symptoms and the patient’s condition. Symptoms may last only a few days, or they may extend for several months. Some people may suffer from chronic pain that lasts for a longer period.
Symptoms of disc herniation vary and may include pain in the back and neck, and muscle spasms. In the case of herniation in the lower vertebrae, the pain may be accompanied by lower extremity pain and feelings of numbness or tingling in the legs or feet. In the case of herniation in the upper vertebrae, the patient may feel pain in the shoulder or arm area and sometimes in the hand and fingers.
In the vast majority of cases, the pain gradually improves over a healing period that extends from several weeks to several months. Complete recovery from disc herniation may take about 3-4 months. However, the patient should continue with the treatment and follow the guidance of the specialist doctor until complete recovery is achieved.
In conclusion, the duration of pain in the case of disc herniation varies from person to person and depends on several factors. Patients are advised to adhere to the prescribed treatment and follow the guidance of the specialist doctor to achieve complete recovery.
How to differentiate between muscle pain and vertebral pain:
Differentiating between muscle pain and vertebral pain is an important matter for many people suffering from back or neck pain. Understanding the difference between these two conditions can help in determining the appropriate treatment and effectively alleviating the pain. Therefore, in this article, we will provide information on how to distinguish between muscle pain and vertebral pain.
Muscle pain:
Muscle strain occurs when a muscle is subjected to stress or injury, and it can result from twisting or tearing of the muscles. Muscle strain can be due to exposure to excessive stress or overload on the muscles. Muscle strain may be accompanied by symptoms such as localized pain in a specific area of the muscle, muscle spasms, and weakness in muscle strength. The pain may increase with movement or when engaging in certain activities that use the affected muscle. The pain can improve after a period of rest and the application of cold and hot treatments and muscle massage.
Vertebral pain:
A disc herniation occurs when there is a tear in the cartilage that covers the vertebrae, leading to a part of the cartilage protruding out of its normal place. Disc herniation may occur as a result of exposure to excessive stress on the vertebrae or overload on the back. Disc herniation can be accompanied by symptoms such as back or neck pain, numbness or tingling in the limbs, and weakness in muscle strength. The pain may increase when performing certain movements or when sitting for long periods. Treatment for disc herniation may require medical intervention such as physical therapy, medication, or in some cases, surgery.
To determine the difference between muscle pain and vertebral pain, a doctor can help by evaluating the patient’s medical history, accompanying symptoms, and performing the necessary examinations such as physical examination and imaging tests like CT scans or MRI.
In general, the treatment for muscle pain and vertebral pain can sometimes be similar, such as rest, applying cold and hot treatments, and muscle massage. However, treatment for vertebral pain may require more specialized medical intervention depending on the patient’s condition.
In summary, it is important to consult a doctor for an accurate diagnosis and to determine the appropriate treatment for the medical condition. Care should be taken to avoid self-diagnosing or relying on unreliable information from the internet.
Can herniated discs be completely cured?
A herniated disc is a common condition that affects the spinal vertebrae, causing painful and bothersome symptoms for patients. Although a herniated disc is a painful condition that can cause muscle spasms and pain in the back and legs, it can be completely cured in some cases.
A herniated disc consists of a part of the nucleus pulposus, which acts as a shock-absorbing cushion between the vertebrae, protruding out when the outer layer of the disc tears and a part of it comes out. This can lead to pressure on the surrounding nerves and spinal cord, causing pain, numbness, and weakness in the limbs.
The degree of recovery from a herniated disc varies based on the patient’s condition, the severity of the herniation, and the duration of the condition. Most patients gradually improve over a period ranging from several weeks to several months. Patients may need rest, physical therapy, and pain-relieving medications to alleviate the symptoms.
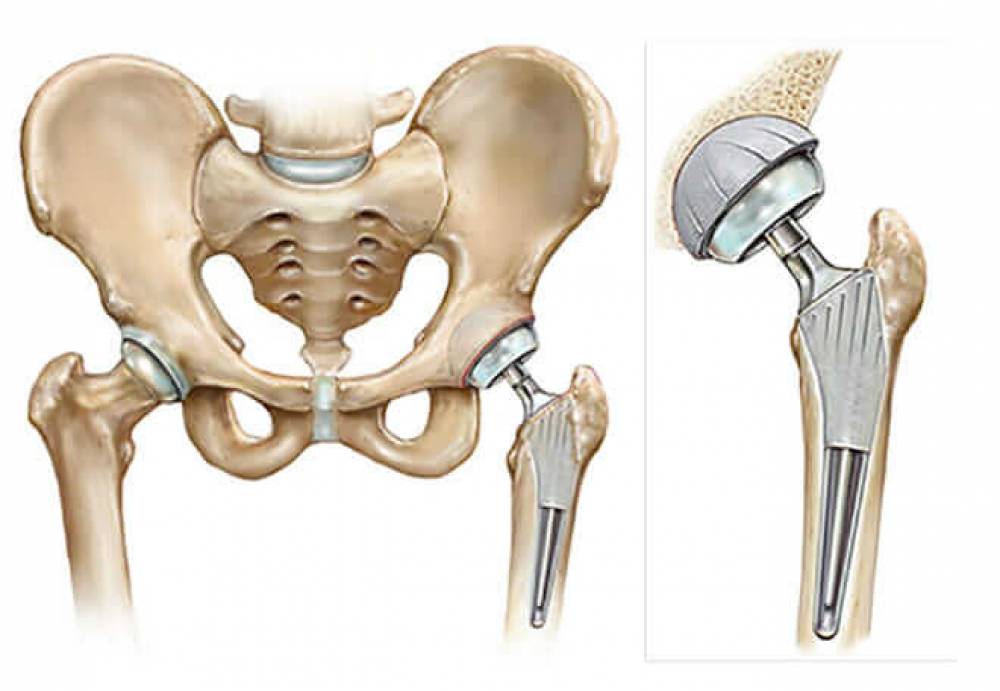
In some severe cases, surgical treatment may be necessary to repair the herniated disc. In this case, the damaged part of the disc is removed and the adjacent vertebrae are re-stabilized. Surgical treatment is another option if the patient does not respond to other treatments or in case of serious symptoms such as muscle weakness or loss of bladder and bowel control.
In addition to medical and surgical treatment, some preventive measures and lifestyle changes can be adopted to alleviate the symptoms of a herniated disc and improve overall recovery. Patients are advised to maintain a healthy weight and practice appropriate exercises to strengthen the core muscles and improve the stability of the spine. Physical therapy, massage, and hot and cold treatments can also be used to relieve pain and improve mobility.
In general, it can be said that a herniated disc can be completely cured in many cases. However, patients should consult a specialist to evaluate their individual condition and determine the appropriate treatment for them. Patients must adhere to prescribed treatments and follow medical guidance to achieve the best healing results.
How do I know if I have a disc in my back?
Back disc is a common condition that many suffer from in our current era, and prolonged sitting, computer use, and incorrect movements we make may be the main reason for developing this disease. Therefore, it is important to recognize some of the signs and symptoms that may indicate the presence of a disc in the back.
One of the most prominent symptoms that may indicate the presence of a disc in the back is pain. The affected person may feel a sharp pain in the back area, which may also extend to the legs. The patient may feel tingling, pain, and a burning sensation at the injury site. The pain may increase during long periods of sitting or when making certain movements.
In addition to pain, the patient may experience other symptoms such as muscle weakness and limb numbness. The patient may feel weakness in the legs or feet and may also experience numbness in the fingers or lower extremities. These symptoms can lead to difficulty in movement and performing daily activities.
To confirm the presence of a disc in the back, the patient should consult an orthopedic or neurologist. The doctor will assess the symptoms and conduct a comprehensive examination of the back. It may also require additional tests such as X-rays or magnetic resonance imaging (MRI).
Magnetic Resonance Imaging (MRI) technology is considered one of the best methods for diagnosing a herniated disc in the back. This technique helps determine the location of the slipped disc and the affected nerves. It also assists in identifying the fissures present in each disc.
After diagnosis, the doctor will develop a suitable treatment plan for the patient’s condition. Treatment may include several options such as medication, physical therapy, massage, and appropriate exercise. In more advanced cases, surgery may be necessary to repair the slipped disc and alleviate symptoms.
To prevent a herniated disc in the back, the spine must be given plenty of attention and necessary care. It is advisable to lift objects safely and correctly, maintain a healthy lifestyle, and regularly practice sports activities. It is also important to avoid sitting in the same position for long periods and to avoid incorrect movements that put pressure on the spine.
In summary, a back disc is a common condition that can significantly affect people’s lives. To ensure the presence of a herniated disc, one must consult a specialist and undergo the necessary examinations. It is also necessary to follow the mentioned prevention guidelines to avoid this disease and maintain spinal health.
What is the difference between a herniated disc and sciatica?
A herniated disc and sciatica are two medical conditions that affect the spine and cause pain in the back and leg area. Although the symptoms may be somewhat similar, there are important differences between them.
A herniated disc, also known as a disc, occurs when the gel-like part inside the spinal discs breaks out and presses on the surrounding nerves. A herniated disc causes sharp pain in the back and leg area, which may be accompanied by a feeling of numbness or tingling in the leg. The pain can be temporary or chronic and may require long-term treatment.
Sciatica, on the other hand, refers to symptoms resulting from pressure or inflammation of the sciatic nerve, which extends from the spine to the leg. Sciatica causes sharp pain in the back area that extends across the leg and may be accompanied by muscle weakness and numbness in the foot. Sciatica can be a result of a herniated disc, but it can also occur due to other reasons such as spinal canal stenosis or slippage of the vertebrae.
The main difference between a herniated disc and sciatica lies in the fundamental cause of the pain and symptoms. A herniated disc occurs when the gel-like part of the spinal disc breaks out and presses on the nerves, while sciatica results from pressure or inflammation of the sciatic nerve.
Although the symptoms may be similar, there are different ways to treat the two conditions. Sciatica is usually treated in a short period using conservative treatments such as physical exercises, physical therapy, and pain-relieving medications. Conversely, a herniated disc requires long-term treatment, which may include physical therapy, anti-inflammatory medications, intensive exercises, and in some cases, surgery.
To protect the back and reduce the risk of sciatica, one can follow some general guidelines such as maintaining good body posture while sitting and standing, avoiding heavy lifting and sudden movements, and performing appropriate sports exercises to strengthen the back and gluteal muscles.
Generally, it is necessary to consult a doctor to diagnose the condition properly and determine the appropriate treatment. Additional tests such as X-rays or MRI may be required to determine the extent of the impact of a herniated disc or the pressure on the sciatic nerve on the nerves.
In summary, a herniated disc and sciatica are two different conditions that cause pain in the back and leg area. Although the symptoms may be similar, they differ in cause and treatment methods. It is essential to consult a doctor to diagnose the condition correctly and determine the appropriate treatment.
What are the causes of a herniated disc?
A herniated disc is a condition that occurs when the cartilage between the vertebrae in the spine tears. The cartilage serves to provide cushioning and balance between the vertebrae and to reduce friction between them during movement. However, cartilage damage can result from many different reasons.
One common cause of a herniated disc is lifting heavy objects improperly. When objects are lifted incorrectly, the cartilage can be subjected to excessive pressure and tear. Therefore, people should learn how to lift objects correctly using the strong muscles in the legs and buttocks instead of the back.
Weakness in the neck or back muscles can also be a cause of a herniated disc. Muscle weakness may be due to genetic or acquired factors such as insufficient physical activity or sitting for long periods without movement. When muscles are weak, they do not provide sufficient support for the spine, increasing the likelihood of cartilage tearing.
Aging is another factor that can increase the risk of a herniated disc. Over time, the cartilage becomes less flexible, and its endurance decreases. This means that it becomes more prone to tearing and damage.
Excessive obesity is another factor that can increase the likelihood of a herniated disc. Excess weight puts extra pressure on the spine and cartilage, making them more prone to damage and tearing.
To prevent a herniated disc, it is advisable to follow some preventive measures. People should be careful to lift heavy objects correctly and use the strong muscles in the legs and buttocks. It is also recommended to exercise regularly to strengthen the muscles of the back and neck. Maintaining a healthy weight through a balanced diet and regular physical activity is also advised.
Overall, people should take care to maintain the health and safety of the spine and avoid factors that may increase the risk of a herniated disc. In case symptoms of pain, numbness, and weakness in movement appear, it is necessary to consult a doctor to diagnose the condition and prescribe the appropriate treatment.
Best Doctor for Endoscopic Disc Herniation Surgery
Dr. Amr Amal is one of the top specialists in endoscopic disc herniation surgery in Egypt. He practices at Dar Al Fouad Medical in room 418 on the fourth floor and is known for his extensive experience and advanced skills in this field.
Endoscopic disc herniation surgery is a surgical procedure used to treat damaged discs between vertebrae to alleviate pain and restore mobility to the affected individual. This technique is among the latest used in Egypt and has been considered one of the most successful in recent years.
The procedure is performed using an endoscope, which allows the doctor to precisely access the affected area without the need for open surgery. The damaged disc is removed and the pressure on the nerves is relieved, which helps in reducing pain and improving the patient’s mobility.
This operation is completely safe and does not require a long recovery time. After the surgery, the patient can resume normal daily activities after only a few days. Patients are advised to avoid strenuous activities in the early recovery period and to follow the treating doctor’s instructions regarding taking pain medications and maintaining complete rest.
The cost of the endoscopic disc herniation surgery is determined by the choice of the treating doctor and the hospital or medical center. Patients should contact one of the best medical centers in Egypt that specialize in endoscopic disc herniation treatment to learn more about the prices and details related to the procedure.
Those affected should take care of their health and seek the best specialists in this field. Dr. Amr Amal is one of the trusted and experienced doctors in endoscopic disc herniation surgery. Patients can rely on him for appropriate and professional healthcare.