What Is Lumbar Disc Herniation, and Does Massage Help with Lumbar Disc Herniation?
أخر تحديث :

What Is Lumbar Disc Herniation?
Lumbar disc herniation is a condition that affects the spinal column, where the discs between the vertebrae in the lower back slip out of place. These discs contain a gel-like substance surrounded by a tough fibrous ring. The outer ring of the disc can experience wear and tear due to aging or repetitive motions that put a lot of pressure on the discs. In some cases, the outer ring may bulge or rupture, causing the inner gel-like substance to press against the nerve roots in the lower back.
Several factors contribute to lumbar disc herniation. Among these factors, lifting heavy objects with improper back bending and experiencing traumatic shocks to the back can be significant. Gender also plays a role, as males are more susceptible to this condition than females. Prolonged periods of driving and extended periods of sitting can also increase the risk of lumbar disc herniation. Additionally, vibrations from a vehicle’s engine and road conditions can put extra stress on the discs.
Symptoms of lumbar disc herniation can range from severe pain to numbness and tingling in the leg or foot. Patients may experience intense pain radiating from the buttocks down to the back of one leg, which is caused by the pressure of the herniated discs on the sciatic nerve. Patients may also feel numbness or tingling sensations in the leg or foot.
In most cases, the pain persists for several days and gradually subsides. However, patients should seek appropriate treatment to alleviate pain and improve their condition. The treatment of lumbar disc herniation depends on the severity of the injury and the patient’s symptoms. Treatment may include pain relievers and anti-inflammatory medications, physical therapy to strengthen the muscles around the spine, and gradual therapy to improve flexibility and strength. In advanced cases, surgery may be required to relieve pressure on the nerves.
In summary, lumbar disc herniation is a common condition that affects the spinal column, where the discs between the lower back vertebrae slip out of place. This displacement results in symptoms such as severe pain and numbness and tingling in the leg or foot. This condition can be treated with medications, physical therapy, and in advanced cases, surgery.
Does Massage Help with Lumbar Disc Herniation?
Massage therapy can be beneficial for some individuals with lumbar disc herniation, but it’s essential to approach it with caution and consult a healthcare professional before starting any massage regimen.
Massage can help in the following ways:
- Pain Relief: Massage can provide temporary relief from pain associated with lumbar disc herniation. It can relax muscles, improve blood circulation, and release endorphins, which are natural pain relievers.
- Muscle Relaxation: Massage can help relax tight muscles around the affected area, reducing muscle spasms and tension that may contribute to pain.
- Stress Reduction: Chronic pain can lead to stress and tension. Massage can promote relaxation and reduce stress, which may indirectly alleviate pain.
- Improved Mobility: Massage can enhance flexibility and range of motion, making it easier to perform physical therapy exercises and maintain mobility.
However, it’s crucial to consult a healthcare provider or physical therapist before getting a massage for lumbar disc herniation. Not all massage techniques are suitable for this condition, and certain techniques or pressure applied incorrectly can worsen the condition. A qualified massage therapist should have experience in dealing with patients with lumbar disc herniation and work in conjunction with other healthcare providers to develop a comprehensive treatment plan.
In conclusion, massage therapy can be beneficial for individuals with lumbar disc herniation in terms of pain relief, muscle relaxation, stress reduction, and improved mobility. However, it should be used as part of a comprehensive treatment plan under the guidance of healthcare professionals who specialize in this condition.
What Are the Symptoms of Lumbar Disc Herniation?
Lumbar disc herniation is a common condition that affects the lumbar vertebrae in the spinal column. This condition occurs when the lumbar discs in the spinal column slip out of their natural position. These discs, which act as shock absorbers and provide flexibility and proper movement to the spine, can slide out of place.
The symptoms of lumbar disc herniation can vary and may differ from person to person, but some of the prominent symptoms that may appear include:
- Sciatica: This is severe pain that radiates from the buttocks down to the back of one leg. It is caused by the pressure of the herniated discs on the sciatic nerve.
- Numbness or tingling in the leg or foot.
- Pain in the lower back, buttocks, and down the back of the leg.
- Muscle weakness in the affected leg.
- Difficulty in controlling the movement of the affected leg.
It’s worth noting that if the condition does not improve after a period of treatments, surgical intervention may be considered as a last resort.
What Is the Treatment for Lumbar Disc Herniation?
Lumbar disc herniation is a condition where the disc in the spinal column slips out of its natural position, causing pain and numbness in the limbs and potentially affecting a person’s mobility. It is a common problem and can occur in any part of the spinal column, but it is most common in the neck and lower back.
There are several methods for treating lumbar disc herniation, including:
- Physical Therapy: Physical therapy involves a set of exercises and measures aimed at relieving pain and strengthening the muscles surrounding the spinal column. Stretching exercises are performed to maintain muscle flexibility, and muscle-strengthening exercises are used to support the vertebrae and discs. Electrical devices may also be used to stimulate muscles and relieve pain.
- Medication: For mild to moderate cases of lumbar disc herniation, medications can be used to alleviate pain and associated inflammation. Medications may include non-steroidal anti-inflammatory drugs (NSAIDs) and pain relievers.
- Interventional Therapy: In severe cases of lumbar disc herniation that do not respond to physical and medical treatments, interventional procedures may be required. These procedures may include localized steroid injections to reduce pain and swelling. In some cases, surgery may be necessary to repair the damaged disc.
Individuals should be evaluated on a case-by-case basis to determine the appropriate treatment. Consulting a specialized physician is often necessary to identify the right steps for treating lumbar disc herniation. Lifestyle changes, such as avoiding strenuous physical activity and maintaining a healthy weight, should also be considered, along with appropriate exercises to strengthen the muscles.
It is essential to prioritize the health and safety of patients and provide them with the latest medical techniques and services for the treatment of lumbar disc herniation. Seeking specialized and certified medical centers is crucial to receiving the necessary care and medical advice.
In conclusion, individuals experiencing symptoms of lumbar disc herniation should adhere to the prescribed treatment and follow the guidance of their treating physician. Improvement may take some time, but with the right approach, many individuals can find relief from the symptoms of this condition.
Can Lumbar Disc Herniation Heal Without Treatment?
Lumbar disc herniation, also known as a slipped disc or disc herniation, is a condition related to the displacement of the lumbar intervertebral disc in the spinal column. Lumbar disc herniation typically occurs when the intervertebral disc, the cushion-like structure between two vertebrae, separates and exerts pressure on the surrounding nerves, leading to pain.
It is challenging to determine whether lumbar disc herniation can heal without treatment, as the response varies from person to person. In some mild cases, symptoms may improve, and pain may be reduced through self-care measures and guided movements. However, in more severe cases that cause chronic symptoms and significantly impact daily life, treatment may be necessary.
The goals of treatment for lumbar disc herniation include pain and inflammation relief, improvement of spinal mobility, and strengthening and stretching of the muscles surrounding the spinal column. The treatment plan may encompass a variety of measures and techniques, including:
- Rest and limitation of activities that exacerbate pain.
- Application of ice or heat to alleviate pain and inflammation.
- Taking pain-relieving and anti-inflammatory medications.
- Undergoing physical therapy sessions to enhance muscle strength and spinal flexibility.
- Engaging in rehabilitation exercises to improve balance and muscular stability.
- Using medical devices like spinal support belts to reduce pressure.
In some severe cases, surgical treatment may be required for lumbar disc herniation. The decision for surgery is typically made by the physician based on the specific characteristics of the condition, the severity of symptoms, and their impact on the patient’s daily life.
In general, early detection and accurate diagnosis are key to successful treatment of lumbar disc herniation. Patients should consider seeking medical evaluation and treatment if they experience persistent or worsening symptoms.
However, in most cases, lumbar disc herniation is not serious and can be treated with non-surgical measures. Treatment often includes rest, avoiding activities that exacerbate pain, taking pain-relieving medications, and physical therapy to strengthen the muscles around the back and improve flexibility.
Additionally, some preventive measures can be followed to reduce the risk of lumbar disc herniation. It is recommended to maintain a healthy weight, regularly engage in exercise to strengthen muscles and improve flexibility, avoid prolonged sitting without movement, and maintain proper posture when sitting and standing.
In general, it is advisable to consult a doctor if you experience any unusual symptoms or if the pain worsens and affects daily life. A physician can evaluate the condition and determine the appropriate treatment and guide the individual to receive the necessary care.
In summary, lumbar disc herniation can be painful and bothersome, and in some cases, it can be serious. It is important to seek medical advice and follow preventive measures to reduce the risk of lumbar disc herniation and maintain back health.
Can Lumbar Disc Herniation Cause Paralysis?
Lumbar disc herniation occurs when the disc between the vertebrae in the spinal column slips. It is a common condition that many people experience and can cause painful symptoms and negative effects on movement and daily functions. But can lumbar disc herniation lead to paralysis?
When lumbar disc herniation occurs, it can affect the surrounding nerves, causing severe pain, numbness, and muscle weakness. In extremely rare cases, lumbar disc herniation can significantly affect the nerves and spinal cord, leading to permanent nerve damage and possibly paralysis. However, it is essential to note that such rare and unusual cases occur only in severe and advanced instances of lumbar disc herniation.
Most cases of lumbar disc herniation do not lead to paralysis and can improve with necessary treatment and proper care. Treatment for lumbar disc herniation includes reducing pain and swelling and restoring spinal mobility. Conservative treatments like rest, ice application, and pain medication may be recommended. Physical therapy and strengthening the muscles surrounding the spinal column can also provide support and stability.
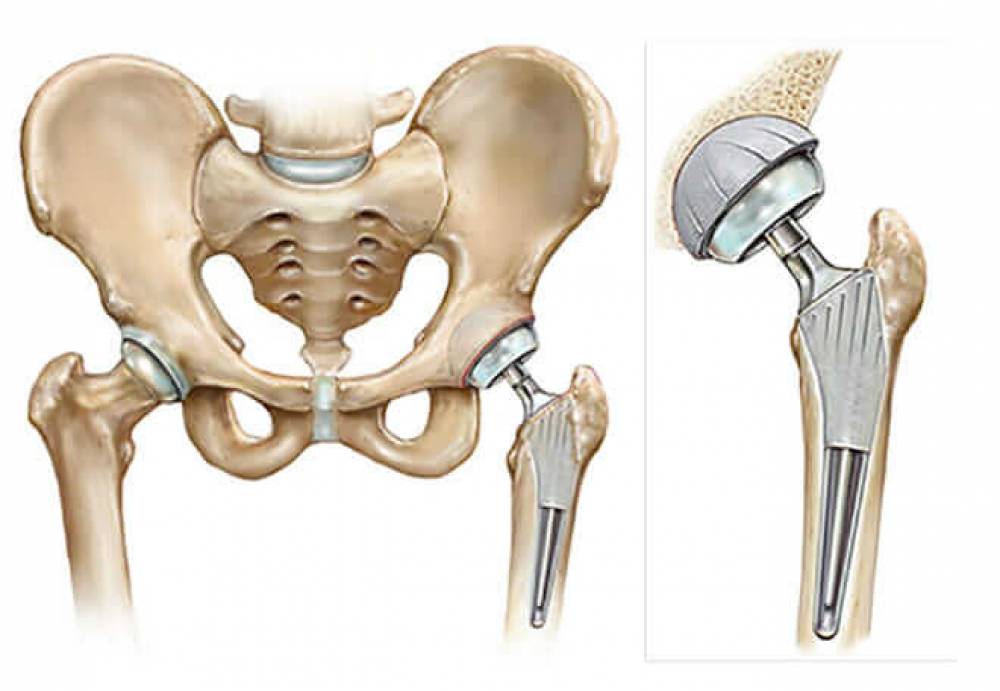
In severe cases of lumbar disc herniation that cause significant pressure on the nerves and spinal cord, surgical treatment may be required. Surgery involves removing the slipped portion of the disc and stabilizing the affected vertebrae to reduce pressure on the nerves and improve symptoms.
In summary, lumbar disc herniation can cause painful symptoms and negative effects on movement and daily functions, and in extremely rare cases, it can significantly affect nerves and lead to paralysis. However, most cases of lumbar disc herniation do not result in paralysis and can improve with necessary treatment and proper care. Individuals experiencing symptoms of lumbar disc herniation should consult a doctor for an evaluation.
Is Massage Beneficial for Lumbar Disc Herniation?
Massage is a therapeutic technique used in the treatment of various health conditions, including lumbar disc herniation. Lumbar disc herniation is a common problem that occurs when the gel-like disc slips between the vertebrae in the spinal column. It can cause bothersome symptoms such as numbness, weakness, stiffness, and limited mobility.
Natural treatments like massage are considered a useful option for patients with lumbar disc herniation. Localized massage is used to alleviate muscle tension and improve the patient’s overall condition. Manual massage therapy involves the use of advanced techniques such as kneading and stretching.
Kneading techniques work to reduce the temperature of the affected muscle, followed by stretching the muscle in opposite directions to reduce tension. These techniques help alleviate pain and improve the patient’s condition.
Additionally, physical therapy works to strengthen the muscles of the back and abdomen, helping to restore mobility and improve spinal alignment. It is important to combine physical therapy with a weight loss program, as excess weight can affect the lumbar spine and delay the patient’s recovery.
However, some important points should be considered before starting massage therapy for lumbar disc herniation. Consulting a specialized physician to evaluate the patient’s condition and determine whether massage is appropriate is necessary. There may be certain cases that require caution in using massage, such as the presence of inflammation or other injuries in the affected area.
In general, massage is considered an effective natural option for treating lumbar disc herniation, as it helps alleviate pain and improve the patient’s condition. However, it is essential to consult a physician.
Is Spondylitis Serious?
Spondylitis is a medical condition that affects the spine and can cause pain, muscle spasms, and limited mobility. Is this condition serious? This is the question that concerns many individuals who suffer from spondylitis. Let’s explore the seriousness of spondylitis and its impact on health.
Firstly, it should be mentioned that spondylitis is a chronic and non-communicable condition, and while it is not life-threatening, it can cause bothersome pain and reduce the ability to move and perform daily tasks.
In some severe cases, the treatment of spondylitis may require surgical intervention to replace damaged vertebrae with artificial ones. However, most cases of spondylitis are managed through non-surgical treatments.
The primary goal of non-surgical treatment for spondylitis is to alleviate symptoms and improve the quality of life. Non-surgical treatment for spondylitis includes the use of medications to relieve pain and relax muscle spasms. Physical therapy and rehabilitation techniques are also used to improve mobility and strengthen the muscles surrounding the spine.
In addition, some tips and lifestyle changes can be followed to alleviate the symptoms of spondylitis. Among these tips are avoiding improper heavy lifting and maintaining a healthy weight. Regular exercise is also recommended to strengthen muscles and improve flexibility.
While spondylitis is not life-threatening, it should be noted that it can worsen over time and impact the quality of life. Therefore, it is important to consult a specialized doctor and initiate appropriate treatment early on.
In conclusion, individuals suffering from spondylitis should be aware of their symptoms and follow the recommended treatment and lifestyle changes. This way, they can control the symptoms and reduce the impact of inflammation.
How Should a Lumbar Disc Herniation Patient Sleep?
Proper and healthy sleep for a lumbar disc herniation patient is essential for the comfort of the lumbar spine and pain relief. The patient should follow some guidelines and proper positions while sleeping to reduce pressure on the vertebrae and improve spinal support. In this article, we will explore some recommended sleeping positions for lumbar disc herniation patients.
Firstly, the patient should sleep on a mattress that is not too soft and on a wooden bed rather than a spring one. The mattress should provide good support for the spine and help distribute weight evenly.
Secondly, it is advised to place a pillow under the head to support the neck and head. The pillow should be elevated enough to align the spine and keep the head level in a straight position.
Thirdly, placing a pillow under the legs to bend the knees is recommended. A pillow can also be placed between the knees if the patient prefers to sleep on their side. This position helps reduce pressure on the lumbar vertebrae and promotes even weight distribution.
Additionally, the patient can try sleeping on their side with the knees bent and a pillow placed between them. This position helps alleviate the curvature in the spine and aids in creating gaps between the vertebrae.
Furthermore, the patient can try sleeping on their back with a pillow placed under the knees. The position should be comfortable and help maintain the curve in the lower spine. This position is suitable for individuals experiencing mild back pain.
Finally, the patient should avoid sleeping on the stomach, as it increases pressure on the lumbar vertebrae and can cause increased pain.
Depending on the preferred position by the patient and the guidance of the doctor, a lumbar disc herniation patient can find the appropriate sleeping position that helps reduce pain and improve the comfort of the lumbar spine. The patient should adhere to these positions and move carefully when changing position to avoid overloading the lumbar vertebrae.
What is the treatment for spondylitis?
Spondylitis is a medical condition that affects the vertebrae in the spinal column, causing pain, stiffness, and limited mobility. The treatment for this inflammation aims to alleviate the symptoms and improve the quality of life and the ability to perform daily tasks.
There are several treatment options available for spondylitis. Medical treatment includes the use of various medications that help manage the pain associated with inflammation. Among these medications, ibuprofen, aspirin, naproxen, and diclofenac can be used.
In addition to medical treatment, the pain and inflammation of spondylitis can be relieved by following some practical tips. It is advisable to maintain a healthy weight and avoid consuming unhealthy foods that can increase inflammation. Also, heavy lifting in the wrong manner should be avoided, and sitting in a proper and comfortable posture for the spine is recommended. There are also benefits to using cold or hot compresses on painful areas.
Physical therapy can also be used to treat spondylitis. This includes exercises to strengthen the muscles responsible for supporting the spine and relieving pressure on the vertebrae and reducing pain. Some individuals benefit from acupuncture therapy, which relies on the use of very fine needles that are inserted into specific areas to increase blood flow, reduce inflammation, and relieve pain.
In cases of severe damage to the vertebrae, surgical intervention may be the optimal solution by replacing the damaged vertebrae with artificial ones. It is important to consult with a specialized doctor if spondylitis is suspected. The doctor can assess the condition and determine the appropriate treatment based on each individual’s circumstances. In the end, patients should adhere to the prescribed treatment and follow medical advice to achieve the best results. Treatment should be comprehensive and holistic.
Best Spinal Column Doctor in Cairo
Dr. Amr Amal is one of the leading and most skilled doctors specializing in spinal column surgery in Cairo. He is distinguished by his high skills and extensive experience in this field, making him the ideal choice for patients suffering from spinal problems.
Dr. Amr Amal holds a master’s degree in orthopedic and joint surgery, specializing in knee joint replacement surgeries. He has also published his research in several journals specialized in orthopedics, reflecting his scientific contribution to this field.
Furthermore, Dr. Amr Amal has obtained a Ph.D. in spinal column surgeries, where he specialized in upper back spinal surgeries. He completed his training in this field in collaboration with the International University of Hong Kong, which enhances his experience and skills in spinal column surgeries. He has also obtained a fellowship from the Swiss Association and underwent distinguished training at Uppsala University in Sweden. Additionally, he obtained the International Fellowship for Spondylitis Research and underwent intensive training at Nottingham University in England and Rush University in Chicago, USA.
In short, Dr. Amr Amal is considered one of the best doctors specializing in spinal column surgery in Cairo. He is characterized by his high academic achievements and extensive experience in this field, working diligently to provide the best healthcare to his patients. If you are suffering from spinal problems, Dr. Amr Amal is the ideal choice for receiving the necessary treatment.