What is Cartilage Pain? And what are the symptoms of vertebral compression on the nerves?

Cartilage Pain
Cartilage pain is a common condition that affects many people around the world. Cartilage is considered one of the main components of the musculoskeletal system and is found in many joints in the body, including the knee, hip, and cervical vertebrae.
Cartilage is characterized by its ability to provide support and balance for the joints, and to absorb and distribute the correct pressure on the bones and surrounding tissues. However, the cartilage can be damaged or irritated due to twisting, excessive mechanical stress, or due to aging.
Cartilage pain is one of the most common symptoms of this condition, and it can be acute or chronic. The patient may feel sharp pain in the affected joint, especially when making specific movements or standing for long periods. Pain may also be accompanied by a feeling of swelling, numbness, and weakness in the affected area.
To diagnose cartilage pain, the patient must visit a specialist doctor and undergo the necessary examinations, including medical consultation, medical history, clinical examination, and relying on diagnostic tests such as MRI.
The methods of treating cartilage pain vary depending on the degree of injury and the patient’s tolerance of symptoms. In mild cases, cartilage pain is treated by rest, avoiding activities that increase pain, applying ice, and taking pain-relieving medications. In more complex cases, surgery may be necessary to repair cartilage damage.
In general, it is advised to maintain a good body posture while sitting and standing, avoid violent movements and excessive strains, maintain a healthy weight, and exercise regularly to strengthen the muscles around the joints and maintain cartilage flexibility.
How do you know if you have a herniated disc?
A herniated disc is a condition that affects the back and spine. It may be difficult to recognize this problem at its onset, as the symptoms may be minor and unnoticeable. However, there are some signs that may indicate that you have a herniated disc.
First, pain is the most common and clear symptom in the case of a herniated disc. When the cartilage slips in the spine, it may put pressure on the surrounding nerves, causing specific pain in the back, neck, hip, and legs. This pain can be constant or intermittent, and it worsens when performing certain activities such as lifting heavy weights or sitting for long periods.
Second, the patient with a herniated disc may experience tingling and numbness in the affected areas. This numbness occurs as a result of the pressure of the cartilage on the nerves, which hinders the transmission of nerve signals and causes this uncomfortable sensation.
A herniated disc may also be accompanied by muscle weakness in the affected area. It may be difficult for the person with a herniated disc to move the affected area due to muscle weakness. This weakness may be especially apparent when trying to perform a specific activity or load the muscles.
In addition, a herniated disc may result in difficulty in movement and bending. The patient feels restricted in their movement, and it may be difficult for them to move easily and flexibly in the affected joint.
Finally, it is not possible to accurately diagnose a herniated disc without undergoing a specialized medical examination. Patients who suffer from the above-mentioned symptoms should seek medical advice to get an accurate diagnosis and appropriate treatment. Remember that early treatment can lead to a significant improvement in symptoms and quality of life.
How do I treat cartilage pain?
Treating cartilage pain can be challenging and discomforting, but there are several steps that can be taken to alleviate pain and promote healing. In this article, we will review some tips that can help you in treating cartilage pain and improving your condition.
Rest and Massage: Relaxing the body and avoiding overexertion can help alleviate pain and reduce inflammation. Gently massage the affected area with circular movements to improve blood circulation and relieve tension.
Muscle Strengthening Exercises: Strengthening the muscles surrounding the cartilage can improve stability and reduce symptoms. Consult your doctor for an exercise program that suits your condition and follow it accordingly.
Stretching and Improving Flexibility: Stretching muscles can help relieve pressure on the cartilage. Try gentle stretching exercises that target the muscles near the problem area.
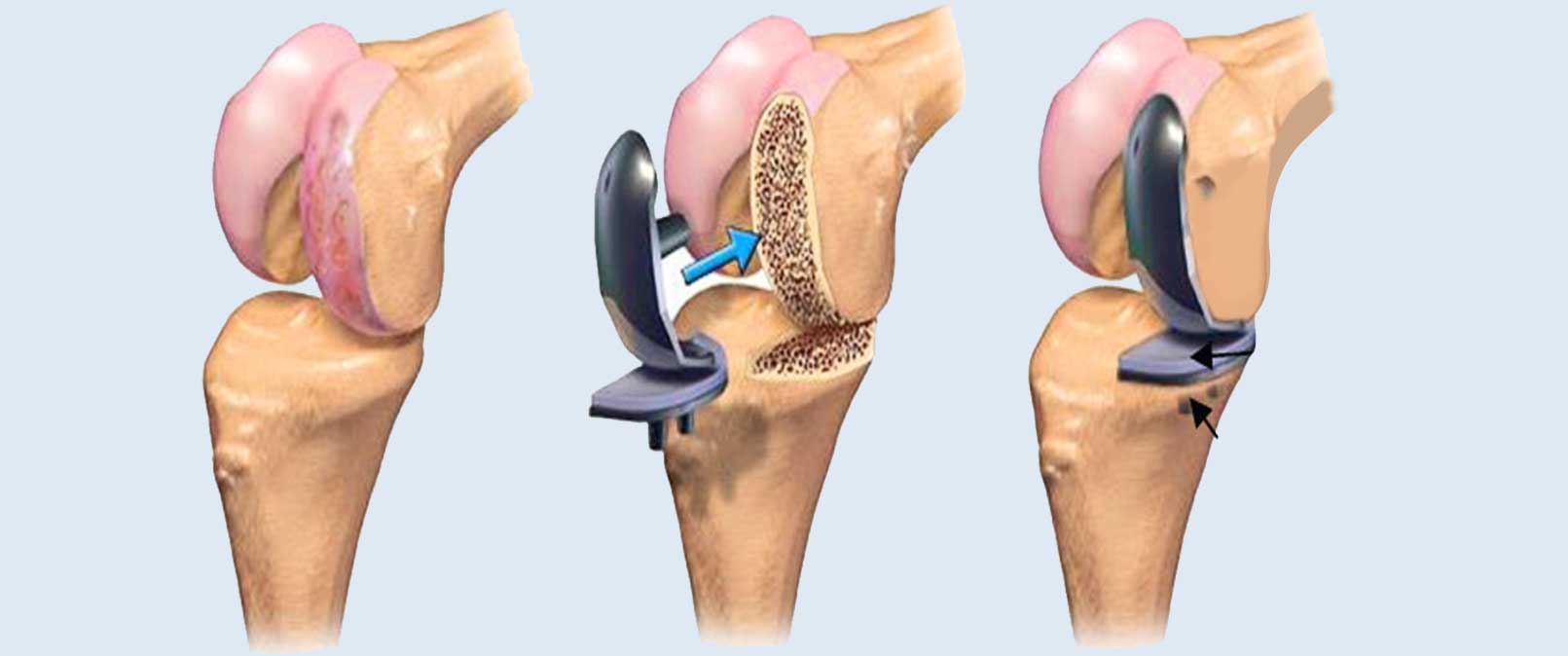
Physical Therapy and Surgical Intervention: In some severe cases, it may be necessary to consult your doctor for other treatment options. This includes physical therapy, massage, and the use of devices that promote healing. In rare cases, doctors may resort to surgery to repair damaged cartilage.
Prevention and Healthy Lifestyle: To prevent cartilage pain or avoid worsening it, it is advisable to avoid activities that put excessive pressure on the joints. It is also recommended to exercise regularly within acceptable limits and use heating and cooling techniques to reduce inflammation.
How many days does the pain of a slipped disc last?
A slipped disc is a common condition that affects many people, causing severe pain and restricting movement. If you are suffering from a slipped disc, here are some tips to help you cope with this condition:
Consult Your Doctor: Before starting any tips or exercises, it is essential to consult your treating doctor to get an accurate diagnosis and a suitable treatment plan. The doctor can guide you properly based on your condition and potential problems you may face.
Rest and Gradual Movement: Give your body enough rest periods to heal. Your doctor may suggest giving you a few days of complete rest and then gradually starting to move slowly. Avoid strenuous physical activities and pressure that can cause further pressure on the damaged cartilage.
Physical Aids: Use physical aids to reduce pressure on the affected cartilage during movement. Tools such as crutches or special shoes can be purchased to provide additional support to the back and legs.
Proper Diet: Eating healthy and balanced food plays an essential role in promoting cartilage health. Include foods rich in calcium and vitamin D in your diet, such as dairy products, yogurt, and healthy proteins like fish and grilled meats. Avoid processed, fatty, and fried foods.
Maintain a Healthy Weight: Maintaining a healthy weight can reduce excess pressure on the cartilage, thus reducing pain and swelling. Follow a suitable diet and exercise routine that fits your condition and physical abilities.
Awareness and Education: Learn more about your condition and how to deal with it. Consult with specialists, online communities, and trustworthy medical websites. This will help you understand more details and find the best strategies to manage a slipped disc.
Coping with a slipped disc can be challenging, but with proper care and advice, affected individuals can improve their quality of life and relieve pain.
How do I treat cartilage pain?
Cartilage pain can be painful and annoying, but there are several steps you can take to alleviate the pain and promote healing. In this article, we will review some tips that may help you treat cartilage pain and improve your condition.
Rest and Massage: Relaxing the body and avoiding overexertion can help relieve pain and reduce inflammation. Gently massage the affected area with circular motions to improve blood circulation and relieve tension.
Muscle Strengthening Exercises: Strengthening the muscles surrounding the cartilage can improve stability and reduce symptoms. Consult your doctor for an exercise program that suits your condition and direction.
Stretching and Improving Flexibility: Stretching muscles can help relieve pressure on the cartilage. Try gentle stretching exercises that target the muscles adjacent to the problem.
Physical Therapy and Surgical Intervention: In some severe cases, it may be necessary to consult your doctor for other treatment options. This includes physical therapy, massage, and the use of devices that promote healing. In rare cases, doctors may resort to surgery to repair damaged cartilage.
Prevention and Healthy Lifestyle: To prevent cartilage pain or avoid exacerbating it, it is recommended to avoid activities that put excessive pressure on the joints. It is also advisable to exercise regularly within acceptable limits and use heating and cooling techniques to reduce inflammation.
How long does the pain from a herniated disc last?
A herniated disc is a common condition experienced by many individuals, resulting in severe pain and restricting the affected person’s movement. If you are suffering from a herniated disc, here are some tips to help you cope with this condition:
- Consult Your Doctor: Before starting any advice or exercises, it is essential to consult your treating physician to get an accurate diagnosis and an appropriate treatment plan. Your doctor can guide you correctly based on your condition and potential issues you might face.
- Rest and Gradual Progression: Give your body enough rest periods to heal. Your doctor might suggest a few days of complete rest followed by gradually increasing movement. Avoid strenuous physical activities and pressure that could cause additional strain on the affected disc.
- Physical Aids: Use physical aids to reduce the pressure on the affected disc during movement. Items like crutches or special shoes can be purchased to provide additional support for the back and legs.
- Proper Diet: Eating a healthy and balanced diet plays a significant role in enhancing the health of the disc. Include calcium and vitamin D-rich foods in your diet, such as dairy products, yogurt, and healthy proteins like fish and grilled meats. Avoid processed, fatty, and fried foods.
- Maintain a Healthy Weight: Keeping a healthy weight can reduce the extra pressure on the disc, thereby lessening the pain and swelling. Follow a suitable diet and engage in exercises that suit your condition and physical capabilities.
- Education and Awareness: Learn more about your condition and how to manage it. Consult with specialists, online communities, and trusted medical websites. This will help you understand more details and find the best strategies to manage a herniated disc.
Living with a herniated disc can be challenging, but with the proper care and advice, affected individuals can improve their quality of life and reduce pain.
Does a herniated disc heal on its own?
A herniated disc is a common condition affecting many individuals of various ages. This condition occurs when the disc between the spinal vertebrae, which works to distribute pressure and absorb shocks, is affected due to deterioration or damage, and it may slip forward, backward, or sideways.
Numerous factors, such as hard work, excessive load on the back, sports injuries, and structural disorders in the spine, can lead to a herniated disc. Despite the pain and spasms caused by the herniated disc, many people wonder whether it can heal naturally or if surgical intervention is required.
In many cases, a herniated disc can heal on its own without needing surgery. The recovery rate depends on the individual’s rest and response to treatment and care. Non-surgical treatment includes strengthening the back and abdominal muscles, applying ice and heat to the affected area, and taking pain relief medications. Some medical devices can also be used to strengthen the muscles and improve the spine’s posture.
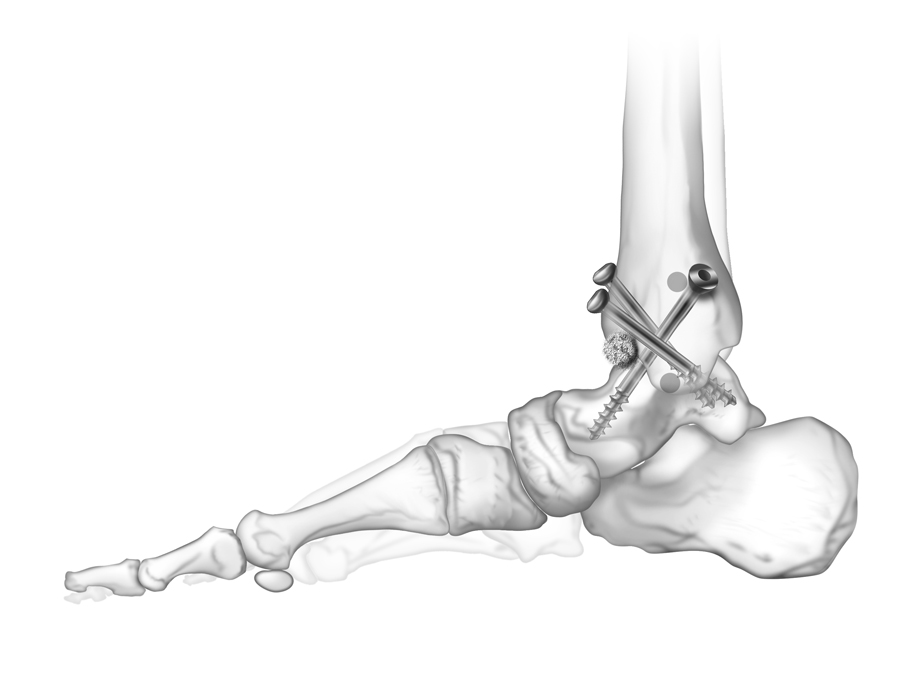
However, in more complex cases, surgical treatment may be necessary. Surgical treatment involves removing the damaged disc, repairing the damaged tissues, and stabilizing the slipped vertebrae if necessary. Although surgical treatment can be effective in repairing a herniated disc, it requires a long recovery period and physical therapy sessions to regain normal movement.
In summary, herniated discs can heal on their own in many cases with non-surgical treatments. However, in more complex cases, surgical treatment may be necessary. It is always advised to consult a specialist to assess the condition of the herniated disc and provide the appropriate treatment.
Tips for those suffering from a herniated disc:
If you are suffering from a herniated disc, you might find yourself in a difficult situation and experiencing pain. But do not despair; there are tips that may help you manage this issue better and alleviate the pain. Here is a list of important tips to help those suffering from a herniated disc:
Choose a good sitting and sleeping posture: Ensure that your sitting position is comfortable and provides support for your spine. Use comfortable and appropriate pillows to ensure back stability and reduce pressure on the disc. As for sleeping, it is preferable to sleep on your side with a pillow of appropriate thickness to support the neck and spine.
Practice appropriate physical exercises: Practicing some physical exercises to strengthen the back muscles and improve the posture of the spine may be beneficial. Consult your doctor or a rehabilitation specialist for guidance on exercises suitable for your condition.
Reduce heavy loads: Try to avoid lifting heavy weights or engaging in intense physical effort, as this type of mechanical load increases the pressure on the spine and can exacerbate herniated disc pain.
Apply heat and cold locally: Applying localized heat or cold to the affected area may be effective in relieving pain and swelling. Use a heat source such as a heating pad or warm bath to warm the affected area, or use ice packs or cold packs for cooling.
Maintain a healthy weight: Pay attention to your weight and try to maintain a healthy weight, as being overweight can increase the pressure on the spine and cause more problems for the herniated disc.
Focus on proper nutrition: Eating foods rich in vitamins and minerals, such as fruits and vegetables, can enhance cartilage health and aid in faster healing.
Consult a physical rehabilitation specialist: Do not hesitate to consult a physical rehabilitation specialist or physical therapist, as they can provide you with appropriate treatment techniques to relieve pain and improve the strength of your back muscles.
Individuals suffering from a herniated disc should remember that these tips are not a substitute for professional medical care. Always consult with doctors and specialists to diagnose your condition and provide appropriate treatment.
Does a herniated disc affect walking?
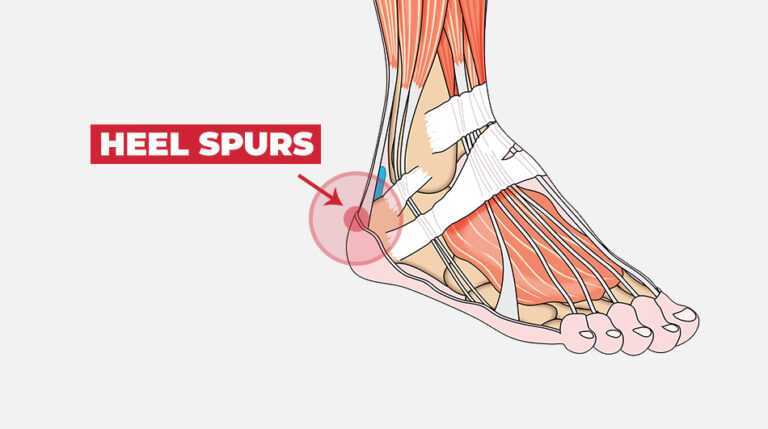
A herniated disc is considered one of the painful and troublesome health issues for many people. It occurs when the cartilage between the vertebrae in the spinal column moves and affects the back nerves. One of the significant side effects of sports collisions and other shocks that the vertebrae face is a herniated disc.
A herniated disc can affect the ability to walk, as it can cause sharp pain that extends to the legs and feet, making normal movement difficult and sometimes impossible. The affected individuals may have difficulty lifting their foot while walking or feel a clicking in the joints, resulting in a reduction in the distance they can walk normally.
In addition, a herniated disc can cause numbness or tingling in the legs and feet and sometimes a loss of sensation. This may lead to impaired balance and an increased risk of falling. People with a herniated disc may find it difficult to walk for long periods and may feel the need to rest regularly to relieve pain and fatigue.
Therefore, people with a herniated disc should take certain measures to minimize its impact on walking. Individuals are advised to maintain good body posture while walking, use assistive devices such as walkers or appropriate shoes to support the natural arch of the foot. Physical therapy is also recommended to strengthen muscles, improve balance, and enhance flexibility.
In general, people with a herniated disc should consult a specialist to determine the best treatment options for them. Treatment may include physical therapy, rehabilitative exercises, physical treatments, and in some severe cases, surgery.
Does a disc herniation cause lower back pain?
A disc herniation is one of the diseases that affect the spinal column, occurring when the intervertebral disc, which acts as a shock absorber for the vertebrae, slips out of place. When this happens, it can affect walking and general movement.
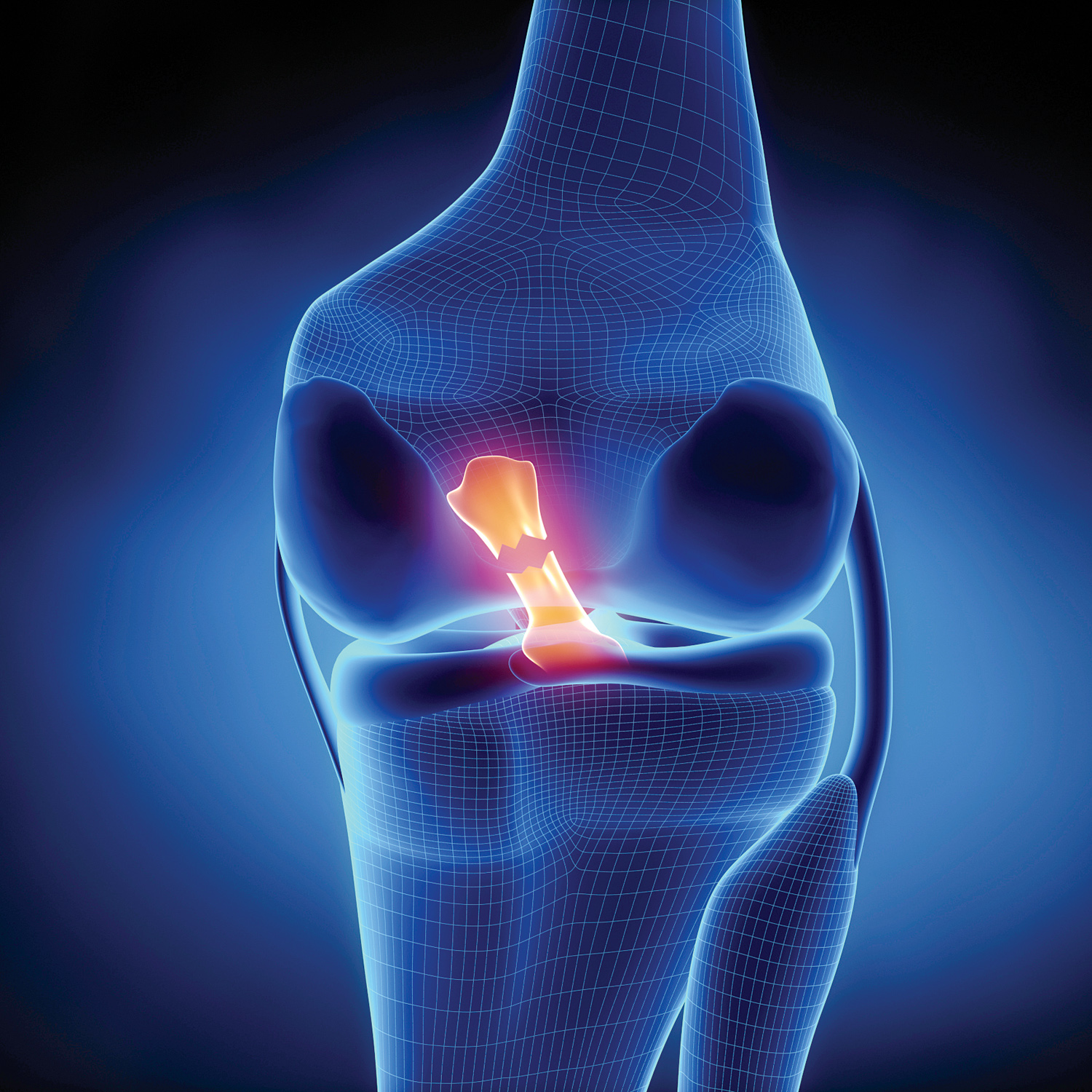
A herniated disc occurs when the intervertebral disc slips from its natural position between the vertebrae. This slippage can cause pressure on the nerves surrounding the spinal column, leading to severe pain and numbness in the legs and feet, and difficulty in moving and walking.
If the herniated disc is mild, it may not have a significant impact on the ability to walk. However, in cases of severe or chronic herniation, the patient may experience difficulty in moving the spinal column and walking normally.
Symptoms of a herniated disc vary from person to person and depend on the extent of the herniation’s impact on the nerves and surrounding tissues. Some patients may experience sharp pain extending from the back to the leg, while others may suffer from muscle weakness and numbness in the extremities.
To treat a herniated disc and improve walking ability, patients are advised to engage in appropriate physical exercises that strengthen the back muscles and enhance flexibility. Prescribed pain relievers and physical therapy sessions can also be used.
Overall, if a herniated disc significantly affects walking ability, doctors may resort to surgical options to address the issue. Surgery involves removing the herniated part of the disc and repositioning it to its natural place.
Does Cartilage Cause Hip Pain?
Cartilage is considered one of the important elements in the human body, as it is found in the body’s joints and contributes to maintaining smooth movement and flexibility. Among these joints, the hip joint is distinguished by the presence of bulging cartilage that plays an important role in providing protection and absorbing shocks during movement.
But can damage or irritation of the cartilage lead to pain in the hip area? The answer lies in the fact that the cartilage itself is not a direct source of pain. Cartilage is a soft and flexible element that separates the bones and acts as an interface for smooth movement, but it does not have nerves for sensing pain.
Therefore, the pain resulting in the hip area may be due to other reasons related to inflammation in the joints adjacent to the cartilage, such as degenerative arthritis (rheumatoid arthritis) or degenerative arthritis resulting from the wear and tear of cartilage with age.
However, damage to the cartilage itself can lead to other complications that can cause pain in the hip area. When the cartilage is damaged, it can lead to abnormal movement of the adjacent bones or excessive friction, which ultimately leads to irritation of the surrounding tissues and pain.
To alleviate pain in the hip area, it is recommended to follow some general guidelines, such as engaging in appropriate physical exercises to strengthen the surrounding muscles and reduce pressure on the hip joint. It is also necessary to refrain from excessively using the affected joints and to avoid excessive movements that may lead to increased pressure on the cartilage and increased pain.
If the pain persists and worsens, the affected individual should visit a specialist doctor to assess their condition, determine the exact cause of the pain, and prescribe appropriate treatment. In some cases, surgery may be necessary to repair the damage or remove foreign bodies causing pain and irritation in the hip area.
Is Ice Beneficial for a Herniated Disc?
A herniated disc is a common medical condition that many people suffer from. It can occur for various reasons, such as exposure to excessive stress on the body or a direct injury to the spine. With the advancement of technology and medical science, there are many methods used to treat a herniated disc, including the use of ice as one of the beneficial means.
Initially, applying ice to the affected area is an effective way to reduce inflammation and pain. When ice is applied, blood flow to the affected area is reduced, which helps in decreasing inflammation and relieving pain. With regular use of ice, it can contribute to reducing the severity of pain and accelerating the healing process. In addition, ice is also beneficial in reducing a herniated disc by improving the muscles’ ability to respond and control. Herniated disc injuries are often accompanied by muscle weakness, leading to loss of balance and an increased risk of injury to the affected area.
When applying ice, the cold can act as a stimulant for the muscles, enhancing their response and control. Therefore, ice can contribute to strengthening the muscles surrounding the spine, thereby reducing the risk of a herniated disc and other future problems.
Despite the benefits of using ice for a herniated disc, it is important to consult a treating physician before using it to know the appropriate time and optimal techniques for application. There may be some cases that require the use of other techniques for appropriate treatment.
What are the symptoms of lumbar vertebrae disease?
Many people may suffer from problems in the spine, and one of these problems is lumbar vertebrae disease, which can cause severe pain and impair the movement of the affected person. Here is a list of the most prominent symptoms associated with this disease:
- Back pain: One of the most prominent symptoms that a person with lumbar vertebrae disease may experience is back pain. The patient may feel sharp and constant pain in this area, and this pain may increase when making certain movements or sitting for long periods.
- Lack of endurance and weakness: Some patients with lumbar vertebrae disease suffer from a lack of endurance, feeling fatigued and tired quickly while performing daily activities. The affected person may also experience general weakness in the muscles.
- Curvature of the spine: Lumbar vertebrae disease may sometimes cause curvature of the spine, affecting the patient’s appearance and causing difficulty in balance and normal movement.
- Numbness and tingling in the limbs: Some people with lumbar vertebrae disease may experience numbness and tingling in the limbs due to the pressure of the disease on the nerves in certain areas of the spine.
- Difficulty breathing: In advanced cases of lumbar vertebrae disease, the deformation of the spine can cause pressure on the nerves and blood vessels adjacent to the respiratory system, leading to difficulty breathing and a feeling of discomfort.
- Muscle cramps: People with lumbar vertebrae disease may experience cramps and spasms in the muscles surrounding the spine. These cramps can be painful and cause restricted movement of the affected person.
Although these symptoms may indicate a problem in the spine, it is best for the disease to be diagnosed and treated by a specialist in this field. Early consultation with a doctor can help alleviate symptoms and improve the quality of life for those affected by this disease.
What are the symptoms of vertebral compression on nerves?
Vertebral compression on nerves is a condition that can occur when nerves in the spine are compressed due to various factors. It can have a significant impact on the nervous system and may lead to the appearance of several uncomfortable and painful symptoms. In this list, we will look at some common symptoms of vertebral compression on nerves.
- Pain in the neck and back: When a nerve is compressed, it may cause sharp or chronic pain in the neck and back. This pain may be constant or may increase during movement of the neck or back.
- Muscle weakness and tingling sensation: When nerves are under pressure, muscle weakness associated with the affected nerve may occur. This weakness may appear as tingling or a numb feeling in specific areas of the body.
- Pain extending to the arms and legs: In case of pressure on the nerves in the neck or back, the pain may extend from the affected area to the arms or legs. The person may experience severe pain or tingling in these areas.
- Dysfunction in nerve function: Vertebral compression on nerves may lead to dysfunction in their normal function. It can cause problems in muscle control or failure of the nerves to transmit signals correctly, resulting in weakness in body sensitivity and movement issues.
- Pressure on the nerve roots: Sometimes, vertebral compression on nerves may cause pressure on the nerve roots exiting the spine. This can lead to severe pain extending to specific areas of the body, such as the arm or leg.
- Changes in sensation: In some cases, vertebral compression on nerves may lead to changes in sensation, such as loss of feeling or increased sensitivity in specific areas of the body.
Remember, if you are experiencing any of these symptoms, it is important to consult a doctor to diagnose your condition correctly and receive the appropriate treatment. Doctors can perform various tests and imaging to determine the location of the vertebral compression and its impact on the nerves.
Best Doctor for Spinal Treatment
If you are suffering from back pain and looking for the best doctor to treat your spinal issues, you are in the right place! Dr. Amr Amal is one of the top specialists in spinal treatments in the Arab world. Dr. Amr Amal has extensive experience in the field of spinal treatments, with his main specialty being spinal surgery. He enjoys an excellent reputation for providing high-quality medical care and effective results for his patients.
Why is Dr. Amr Amal the best choice?
Long Experience: Dr. Amr Amal has a long experience in the field of spinal treatments, having performed numerous successful surgeries for his patients.
Technology Update: Dr. Amr Amal follows the latest technologies and methods for treating spinal issues. He uses a variety of advanced tools and devices to ensure positive results and minimize surgical intervention as much as possible.
Healing and Comfort: Dr. Amr Amal works hard to ensure the complete healing and comfort of his patients. He provides comprehensive treatment programs that include surgery, physical therapy, and lifestyle adjustments to help expedite recovery.
Personal Attention: Dr. Amr Amal treats each patient with care and respect. He listens to their problems and concerns and provides the necessary advice and support throughout the treatment period.
Excellent Reputation: Dr. Amr Amal receives positive evaluations from his patients and colleagues in the medical field. He has an excellent reputation as one of the top doctors for spinal treatments in the Arab world.