Symptoms of Lower Back Disc Herniation and Finding the Best Doctor for Disc Herniation

Symptoms of Lower Back Disc Herniation
The symptoms of lower back disc herniation can be painful and cause a lot of discomfort. However, recognizing these symptoms is crucial for early diagnosis and appropriate treatment. Here is a list of symptoms of lower back disc herniation that should be monitored:
- Back Pain: Patients experience severe pain in the lower back. The pain can be described as throbbing or continuous and may worsen when pressure is applied to the affected area.
- Leg Pain: In addition to back pain, leg pain can also accompany disc herniation. The pain can be sharp and radiate from the lower back through the thigh and down to the knee.
- Difficulty Walking or Standing for Long Periods: Patients may find it challenging to walk or stand for extended periods due to the pain and weakness resulting from disc herniation.
- Numbness or Tingling in the Leg: The pain may be accompanied by numbness or tingling in the right or left leg. Patients may feel as if a needle is entering their foot or leg.
- Leg Weakness: Patients may experience stiffness, numbness, or weakness in the legs or a sensation of stiffness in the lower back. This feeling can be discomforting and affect natural movement.
If you experience any of these symptoms, it is essential to consult a doctor for proper diagnosis and treatment. The doctor may perform a comprehensive examination and use X-rays or magnetic resonance imaging (MRI) to determine the extent of the herniation’s impact on the nerves and surrounding tissues.
In treatment, the doctor may recommend applying heat therapy or physical therapy to alleviate pain and strengthen the muscles around the back. In severe cases, surgical intervention may be necessary. However, it is crucial to avoid practices that may increase the risk of disc herniation. Maintain proper body posture when sitting, standing, and lifting heavy weights. Staying physically fit through appropriate exercise and maintaining a healthy weight is also essential.
What Are Disc Pains?
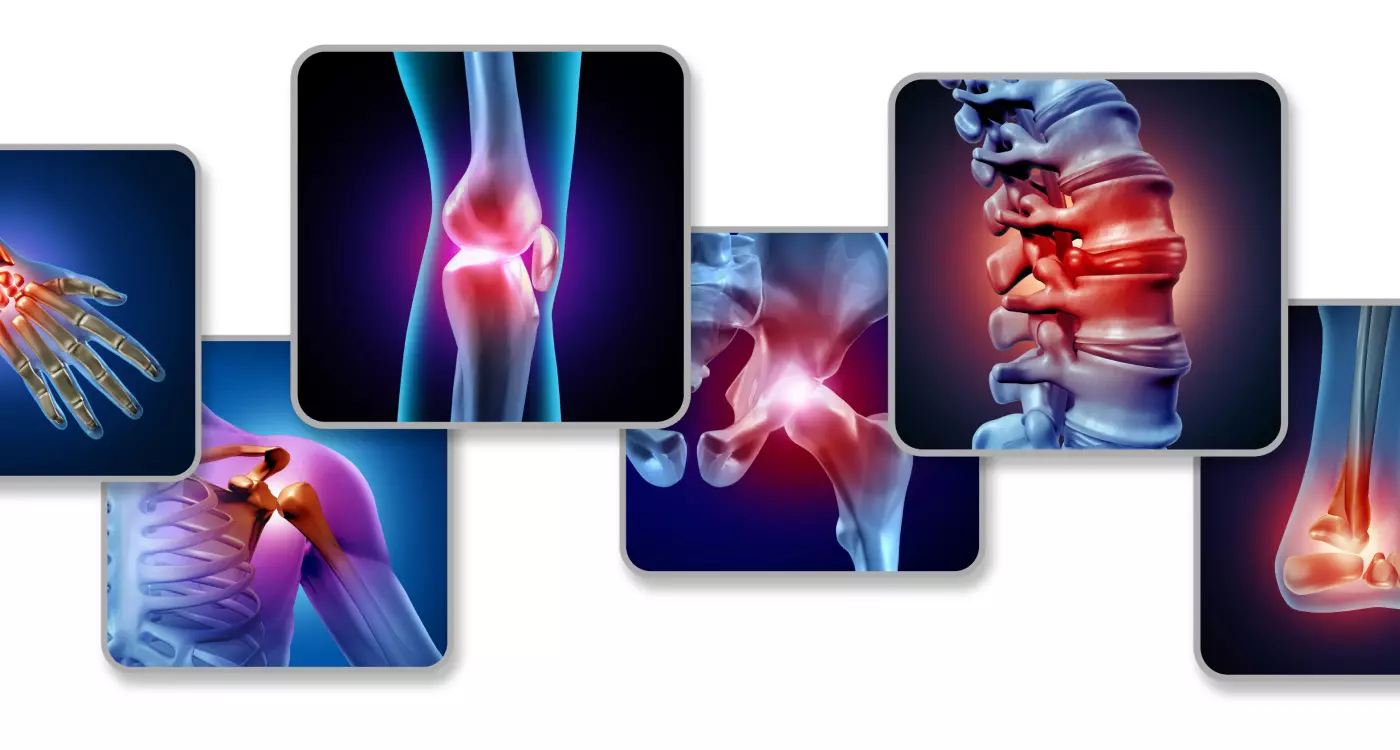
Discs can suffer from various and diverse pains that are considered symptoms of disc inflammation. Pain can be one of the symptoms of disc herniation, resulting in pain that extends from the lower back to the leg if the herniation is in the lumbar region of the spine. In the case of herniation in the cervical region, the patient may feel pain radiating to the arms or shoulders. It is important to consult a doctor if the pain persists and the condition does not improve.
Additionally, disc inflammation may be accompanied by other symptoms such as fever, redness, swelling, numbness, tingling, and a feeling of numbness and stiffness in the joints. Patients may complain of painful swelling in the joints of the fingers, hands, shoulders, elbows, knees, ankles, toes, and pelvis. Disc inflammation can also cause pain in the ribs, throat, or neck.
How Does a Patient with Disc Herniation Sleep?
Sleep plays a crucial role in the comfort of patients suffering from spinal disc herniation. Therefore, it is essential to know the correct sleeping positions to alleviate pain and improve sleep quality. There are several different positions in which patients with disc herniation can sleep properly.
First, it is preferable for the patient to lie on their back with a pillow under their knees. A small pillow or groove can also be placed under the knees to provide the necessary support for the spine and the patient’s comfort. The patient should listen to their body and the pain’s feedback to find a position that does not cause discomfort.
Second, patients can sleep on either side of their body in the fetal position. This position can reduce the curvature of the spine and alleviate pressure on the affected nerves. It is advisable to switch between both sides to balance the muscles on both sides. A pillow can be placed under the neck to provide spine support in this position.
Third, some patients may benefit from sleeping on their stomach. A thin pillow can be placed under the abdomen and hips to improve spinal alignment in this position. Sleeping on the stomach can be helpful for individuals with disc herniation, especially those with a herniated lumbar disc, as it can reduce pressure on the discs.
It is important for patients suffering from disc herniation to consult their treating physician before making any decisions about the appropriate sleeping position. Patients can also consult a rehabilitation specialist or physical therapist for guidance on the best sleeping position based on their health condition and individual needs.
In the end, patients should pay attention to the sleeping position that provides them with pain relief and comfort, ensuring a peaceful and comfortable sleep. Patients should also adhere to the medical advice and recommendations specific to their condition to maintain spine health and reduce disc herniation-related symptoms.
What Causes Lower Back Pain above the Buttocks?
Many women may experience lower back pain above the buttocks, which can affect their ability to sit on the buttocks correctly. Here are some possible causes of this type of pain:
- Coccydynia (Tailbone Pain): Coccydynia is a common cause of lower back pain above the buttocks. This pain occurs due to inflammation or injury to the coccyx (tailbone), which can result from sitting for extended periods without changing position or direct injury to this area.
- Lumbar Spine Issues: Problems in the lower lumbar spine, such as disc herniation or spinal stenosis, can cause pain in the lower back above the buttocks. The pain may be associated with these issues or radiate to the tailbone.
- Rectal or Anal Prolapse: Pain may also result from rectal or anal prolapse in the rectum or anus area. This prolapse can be a cause of severe pain in the lower back above the buttocks.
- Coccygeal Stasis: Coccygeal stasis or fluid-filled cysts in the tailbone region can be a rare cause of lower back pain above the buttocks. Stasis in this area can occur due to the accumulation of fluids or hair.
- Coccygeal Inflammation: Inflammation of the coccyx (tailbone) may also cause pain in the lower back above the buttocks. Coccygeal inflammation can result in sharp and continuous pain in this area, often necessitating consultation with an orthopedic physician.
These are some potential causes of lower back pain above the buttocks in women. If you experience this type of pain, and it persists for an extended period, it is advisable to consult a doctor for necessary examinations and an accurate diagnosis.
Can Back Disc Herniation Be Completely Cured?
- Complete Recovery Is Possible: In cases of simple and uncomplicated disc herniation, patients can fully recover and return to their normal lives after a short period of appropriate treatment and care.
- Gradual Improvement: In most cases, patients experience a gradual improvement in the symptoms of disc herniation over a period ranging from several weeks to several months. Complete recovery may take longer, depending on the characteristics of the condition.
- Non-Surgical Treatment: In many cases, disc herniation is treated using non-surgical methods such as physical therapy, conservative treatment techniques, and lifestyle modifications. Patients may be advised to use medications to alleviate pain, swelling, and inflammation.
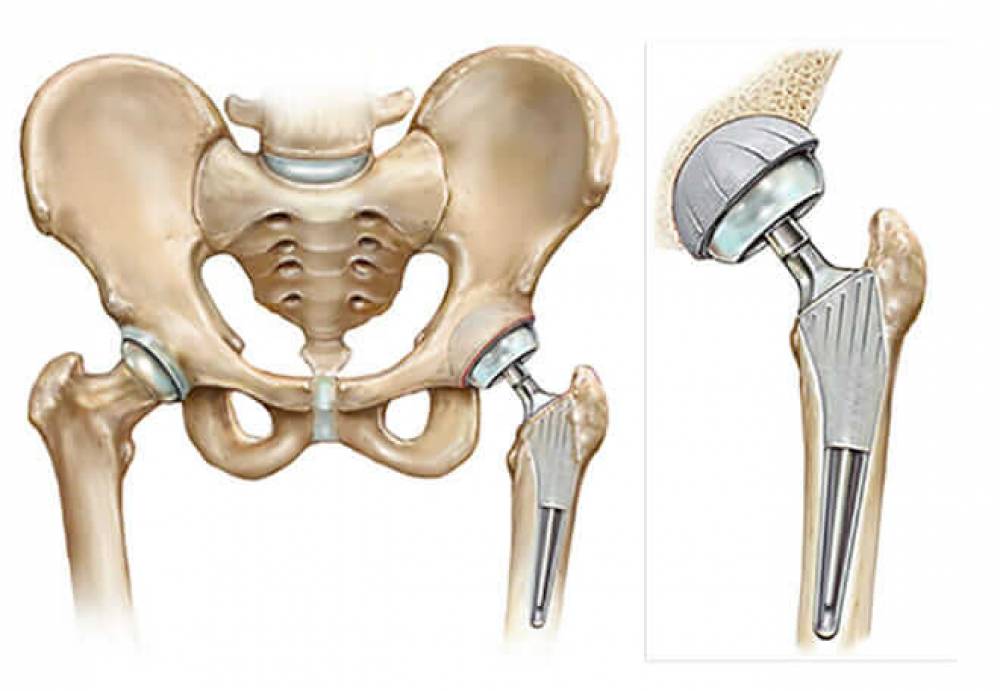
- Surgical Treatment: In some severe cases and when the patient does not respond to non-surgical treatments, surgery may be necessary. The surgery typically involves removing the herniated portion of the disc and relieving pressure on the spinal nerves. After surgery, a rehabilitation program is implemented to strengthen muscles and restore natural movement.
- Prevention and Condition Management: After treatment and recovery, patients should follow the guidance and advice of their doctors to prevent the recurrence of disc herniation. Among these recommendations are maintaining good posture while sitting and standing, strengthening core muscles through low-impact exercises, and avoiding long, excessive movements that strain the back.
Is Sitting Dangerous for Disc Herniation?
Sitting incorrectly can have a detrimental impact on spinal health in general, but is sitting considered dangerous for disc herniation? Absolutely, yes. Disc herniation is a common health condition caused by damage or displacement of the discs between the vertebrae, resulting in severe pain and negative effects on an individual’s daily life. Sitting in the wrong position for extended periods puts abnormal pressure on the discs and joints of the spine, negatively affecting the back and increasing the risk of disc herniation.
When a person sits incorrectly, such as leaning on one arm or leaning to the right or left, the spine bears abnormal pressure. This pressure leads to the deterioration of the discs and their condition, increasing the likelihood of disc herniation. Additionally, sitting in an incorrect position can weaken the muscles surrounding the spine, increasing the risk of other problems such as muscle inflammation and back spasms.
Therefore, it is essential for individuals to be cautious when sitting and to follow some proper guidelines to prevent disc herniation. Important considerations include:
Avoid sitting for extended periods and ensure regular, intermittent movement. Maintain the correct posture for the back while sitting, with back support, and avoid excessive bending. Avoid strong vibrations while sitting, such as off-road driving or riding a motorcycle on rough roads. Engage in specific exercises to strengthen the back and abdominal muscles to improve muscle support and stability for the spine.
How Long Does the Pain from Disc Herniation Last?
The duration of pain resulting from disc herniation can vary from person to person and depends on several factors.
Typically, the pain associated with disc herniation lasts for a period ranging from a few days to a few weeks. In rare cases, the pain may persist for a longer period of several months. The condition should be regularly evaluated and monitored by a specialized doctor to determine the duration of the pain and take appropriate actions.
In addition, self-care measures can be taken to alleviate pain and improve the condition. For example, applying ice to the affected area can help reduce inflammation and pain. Medical rehabilitation methods such as physical therapy or chiropractic treatment can be used to strengthen muscles and improve the flexibility of the spine.
However, patients should consult a specialized doctor if the pain persists for an extended period or if the symptoms worsen, as medical treatment or surgical procedures may be required. Each case should be assessed individually based on the symptoms and accurate medical diagnosis.
Can the Spinal Disc Regenerate Itself?
Can the disc regenerate itself? Discs are considered vital tissues found in various joints in the body, including the spine. They act as flexible cushions that provide balance, shock absorption, and vibration absorption.
While some individuals may experience disc healing to some extent, the regenerative ability of discs is limited and depends on several factors. This includes the degree of injury, the thickness of the damaged disc, and the person’s age.
When a disc is injured, it may experience tears or scratches in its natural softness. While minor damage can potentially heal through a self-repair process, major damage may require additional measures for recovery.
Several factors affect the disc’s ability to regenerate itself. Among these factors is proper nutrition and a suitable diet that provides the necessary nutrients for disc health, such as collagen and essential proteins.
In addition, effective treatment and appropriate exercises to strengthen the muscles surrounding the joints and improve disc function are important. Some individuals may use recommended dietary supplements to enhance disc health and improve its regenerative capacity. Although complete disc regeneration may be challenging, proper care of the discs and adherence to appropriate treatment can help maintain joint health and reduce disc degeneration.
Can Disc Herniation Heal Without Treatment?
Disc herniation poses a health problem that causes a lot of pain and discomfort for affected individuals. Many people wonder whether disc herniation can heal without the need for treatment. The answer to this question depends on each individual’s condition and the severity of the disc herniation they are experiencing.
While disc herniation can improve without the need for treatment, it’s important to take multiple factors into consideration. It’s likely that symptoms will gradually fade over a period typically ranging from several weeks to a few months, and in some cases, it can take up to 3 or 4 months. However, it should be noted that symptoms of disc herniation during this period of improvement can be extremely severe and significantly impact daily activities.
If the symptoms heal and disappear, it does not necessarily mean the disc herniation has fully healed and returned to its normal state. In some cases, the disc may not be able to return to its original condition. Therefore, there is a possibility of symptoms recurring in the future.
From a treatment perspective, there are several options that can be explored to alleviate symptoms and improve the condition. Non-surgical treatment focuses on pain relief and includes pain-relieving medications such as ibuprofen and naproxen. Strengthening exercises for the abdominal and back muscles to support and stabilize the affected vertebrae can also be used.
The Best Doctor for Disc Herniation
Dr. Amr Amal is one of the best doctors in Egypt specializing in the treatment of disc herniation. He holds a Ph.D. in orthopedic surgery from Ain Shams University and is distinguished by his extensive experience and deep knowledge in this field. Dr. Amr Amal’s services in disc herniation treatment focus on using various therapeutic approaches. He offers medical treatment, localized injections, arthroscopic surgery, and various joint-related surgical procedures. He is also a consultant in orthopedic and joint surgery.
Dr. Amr Amal is highly dedicated to the comfort of his patients and places great emphasis on the accurate diagnosis of disc herniation cases and the design of effective and appropriate treatment plans for each case. He always strives to provide optimal care for patients, taking into account the psychological conditions of each individual. Dr. Amr Amal also emphasizes the application of the highest infection control standards within the clinic and has an excellent reputation in the medical sector.