Causes of Herniated Discs and What You Don’t Know About Cartilage Surgery with Thermal Frequency!

Causes of Herniated Discs
Here is a list of causes of herniated discs that individuals should be aware of:
Aging: Aging is one of the main causes of herniated discs. Over time, the cartilage becomes less flexible and less capable of absorbing shocks, making it more prone to tearing and herniation.
Excessive Physical Activities: Engaging in intensive and excessive physical activities can lead to additional pressure on the spinal disc cartilages. This extra pressure may result in herniation, causing pain and discomfort.
Incorrect Ascending and Descending Movements: Incorrect movements when going up and down stairs or slopes can lead to disc herniation. It is advised to maintain proper balance and body alignment during these movements to reduce the risk of herniation.
Obesity: Obesity can increase the risk of disc herniation. Excess weight increases the pressure on the cartilage discs, making them more susceptible to wear and tear and herniation.
Previous Injuries: If you have suffered from a previous spinal injury, you may be at a higher risk for future disc herniation. Past injuries can cause structural changes and weaken the cartilage, increasing the likelihood of herniation later on.
Genetic Factors: Some studies suggest that genetic factors may increase the likelihood of disc herniation. If there is a family history of disc herniation, you may be at an increased risk.
Constant Work in Incorrect Posture: Working for long periods in incorrect postures can increase the risk of disc herniation. Sitting for extended periods with a curved back, or lifting objects incorrectly, can put extra pressure on the cartilage and increase the chances of herniation.
Individuals should remember that these causes are not a fixed rule but are contributing factors that increase the likelihood of disc herniation. It is recommended to follow a healthy lifestyle, engage in appropriate physical exercises, and maintain good posture during work and daily activities to reduce the risk of disc herniation and to maintain the health of the spine.
Is recovery from a herniated disc possible?
A herniated disc is a chronic and common condition in many individuals. This slippage occurs when the cartilage, which acts as a cushion between the vertebrae, is pulled, leading to its outward displacement and resulting pressure on the surrounding nerves.
Several factors can increase the likelihood of a herniated disc, such as sports injuries or accidents, aging, and genetic factors. Lifestyle can also play a role in the occurrence of this slippage, such as standing for long periods or sitting improperly.
In the early stages of a herniated disc, individuals may experience back or neck pain, which can extend to the lower or upper limbs, and may be accompanied by muscle weakness or numbness in the limbs. Those affected by this condition struggle with movement and performing daily tasks normally.
There are various treatment options for a herniated disc, ranging from physiotherapy, massages, and rehabilitative exercises, to surgical treatment in cases where the condition does not respond to other treatments. Recovery from a herniated disc may take a long time, potentially weeks or even months, depending on the individual’s condition and the severity of the slippage.
However, many people fully recover from a herniated disc after appropriate treatment. It is necessary to take precautions to avoid straining the back or spine after recovery and to practice the rehabilitative exercises prescribed by your doctor to maintain back health and prevent recurrent conditions.
What are the prohibited exercises for a herniated disc?
It is known that a herniated disc is a condition suffered by many individuals, and identifying prohibited exercises is an essential part of maintaining vertebral health and reducing the risk of a herniated disc. So, what are these prohibited exercises?
Topping the list are rebounding and high jumping exercises. These exercises place a high amount of pressure on the vertebrae and can increase the risk of a herniated disc. Therefore, such exercises should be avoided. Exercises that require excessive bending and movement of the spine are also prohibited. Excessive bending can cause wear and damage to the disc, increasing the risk of slippage. Thus, exercises involving intense back bending should be avoided.
Heavy weightlifting exercises are also considered prohibited for those with a herniated disc. These exercises increase pressure and tension on the vertebrae, significantly raising the risk of slippage. Therefore, it is preferable to avoid lifting heavy weights when suffering from a herniated disc. Additionally, one should avoid repetitive exercises that increase the impact shocks on the vertebrae, such as motorcycle riding or jumping from high places. These exercises make the vertebrae more prone to injury and damage.
It is crucial for individuals with disc problems to understand that excessive friction and pressure on the vertebrae can exacerbate the issue and increase the risk of a herniated disc. Therefore, it is important to consult a specialist before engaging in any exercise to avoid negatively impacting back health.
How do you know if you have a herniated disc?
A herniated disc can be very painful and uncomfortable, but how can one know if they are suffering from it? There are several signs that may indicate a person has a herniated disc.
A decrease in movement and the ability to perform daily activities easily is one of the main symptoms of a herniated disc. A person suffering from this problem might find it difficult to move or sit for long periods, and severe pain may emanate from the affected disc area.
Issues related to daily routine tasks could also be a sign of a herniated disc. For example, a person might find it difficult to lift heavy objects or perform simple household chores. They might also experience pain in certain movements or positions, such as sitting back on a chair or sleeping on the affected side.
Another potential sign of a herniated disc is numbness or tingling in the lower extremities. The pain can intensify in the thigh, knee, or foot and is sometimes associated with numbness or tingling.
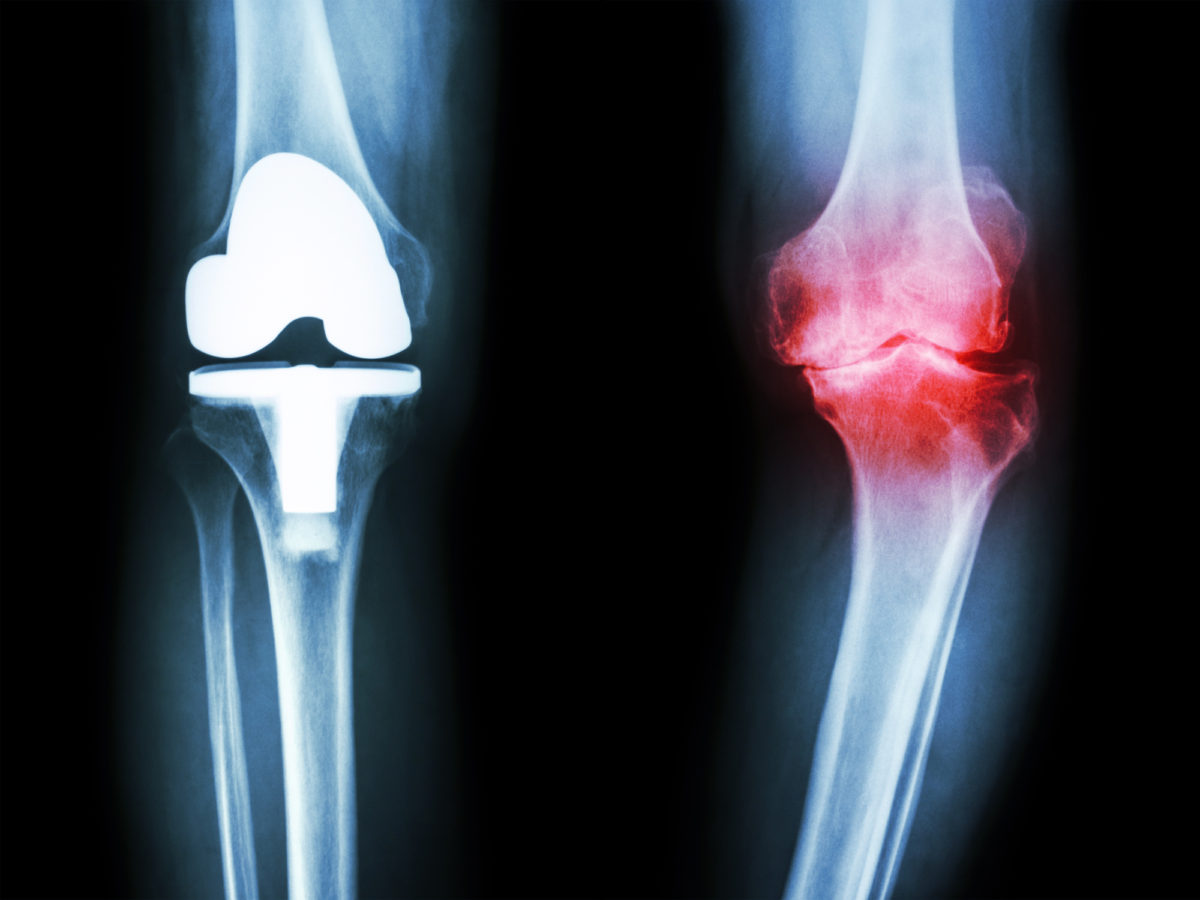
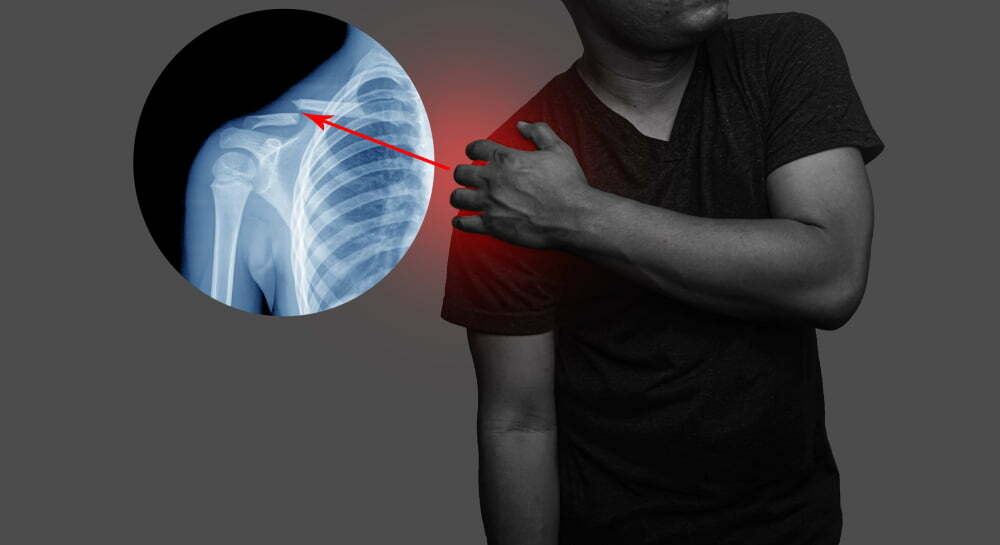
X-ray examinations and magnetic resonance imaging (MRI) are considered the most effective means for diagnosing a herniated disc. X-ray can determine the size of the gap between the vertebrae and diagnose the condition of the disc, while MRI is used to view the anatomical structure of the spine in greater detail.
It is important to contact a doctor if there are symptoms indicating the possibility of a herniated disc. The person may be referred to an orthopedic specialist or a physician to assess their condition and provide appropriate treatment. In some cases, surgery may be recommended to repair the herniated disc and restore the normal functions of the spine.
Tips for those suffering from a herniated disc
If you are suffering from a herniated disc, you might be eager to know tips that help alleviate symptoms and improve your overall condition. Here are some tips that you can follow to deal with this problem:
Regular exercise: Engaging in appropriate physical exercises is an important part of managing a herniated disc. It is recommended to perform exercises that strengthen the muscles around the disc, such as accumulative exercises and stimulative exercises for strength and coordination.
Maintaining a healthy weight: Being overweight is associated with increased pressure on the disc, increasing the likelihood of worsening symptoms. Therefore, it is essential to maintain a healthy weight through proper nutrition and regular physical activity.
Adopting good posture: Be sure to sit and stand in the correct posture to maintain back alignment and reduce pressure on the disc. It is advisable to sit on a comfortable chair and use cushions for support if needed.
Avoiding excessive movements: Avoid excessive movements that put extra pressure on the disc, such as lifting heavy weights or exposure to strong impacts. It is also preferable to avoid deep seats or soft beds that may increase the likelihood of abnormal spinal movement.
Applying healthy practices in daily life: It is important to pay attention to overall health and apply healthy methods in daily life. This includes maintaining mental and physical balance and ensuring adequate rest and good sleep.
Remember that the above tips are general recommendations, and it is essential to consult a specialist doctor before taking any action to treat a herniated disc. The doctor may provide additional advice or direct you to other treatments that suit your specific condition.
Does the Intervertebral Disc Herniation Progress?
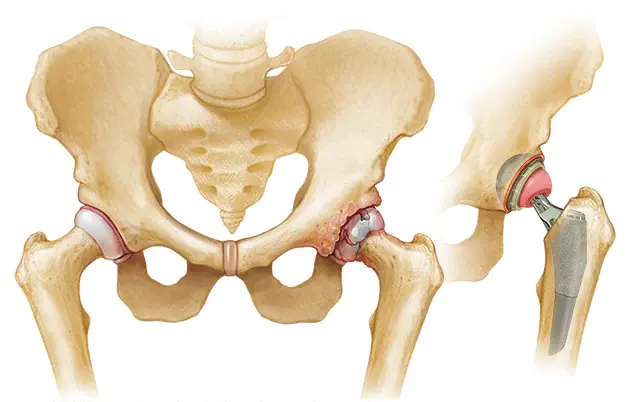
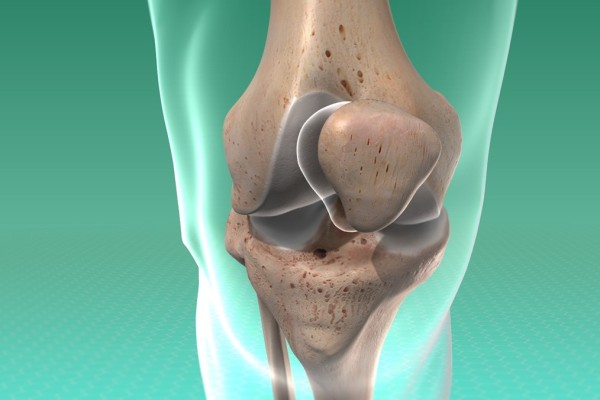
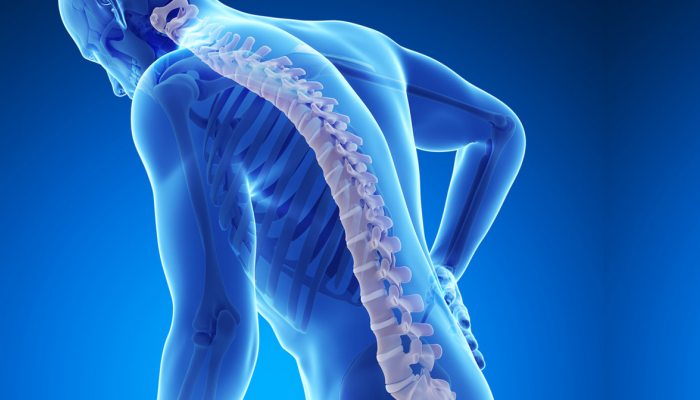
The intervertebral disc herniation is considered a common problem affecting the cartilage in the spinal column. The cartilage acts as a thin and soft layer located between the vertebrae of the spinal column, functioning to reduce friction and absorb shocks during the movement of the spinal column.
When a disc herniation occurs, the cartilage may shift from its usual position and press on the nerve roots or surrounding nerves. This pressure can cause severe pain and numbness in specific areas of the body.
Studies indicate that intervertebral disc herniation may be a result of several factors, including the gradual deterioration of the cartilage with aging, exposure to stress, and repeated injuries to the spinal column, as well as a deficiency in vitamin D.
Nevertheless, despite the pain and discomfort caused by intervertebral disc herniation, it is considered a manageable condition. There are various treatments available to help patients alleviate symptoms and reduce the swelling and inflammation associated with disc herniation.
Initial treatment for disc herniation usually requires some rest and avoiding activities that increase back pain. Pain relievers and anti-inflammatory medications may also be taken to alleviate symptoms.
If symptoms do not improve, physical therapy may be recommended to strengthen back muscles and improve flexibility, as well as heat and cold therapy to relieve pain. More severe cases may require surgery to repair or remove the damaged cartilage.
In general, the improvement of intervertebral disc herniation depends on several factors, such as the severity of the condition, the duration of the injury, and the type of treatment followed. Improvement in disc herniation cases often occurs after a period of treatment and necessary care. However, proper nutrition and appropriate physical exercise can play a significant role in strengthening the spinal column and preventing future disc herniation.
Is Sciatica the Same as Intervertebral Disc Herniation?
Diseases affecting the spinal column are among the most common in our society today. One of these conditions is known as intervertebral disc herniation, which causes severe pain and restricts the movement of the affected individual. However, an important question may arise among some about whether sciatica is directly related to intervertebral disc herniation or not.
Sciatica is a condition where the person suffers from lesions or separations in the long muscular disc fibers in the spinal column. This condition leads to excess pressure and friction on the spinal columns, causing sharp pain and potentially affecting the individual’s normal movement.
On the other hand, intervertebral disc herniation is a condition where one of the discs – the cushions between the spinal column vertebrae – slips and presses on surrounding nerves, causing sharp pain and restricting the individual’s movement.
Although sciatica and intervertebral disc herniation may share some symptoms such as pain and discomfort in movement, there are fundamental differences between them. Sciatica occurs due to damage or separation in the muscular disc fibers, while disc herniation occurs due to a slipped disc. Moreover, sciatica may result from irritation of nerves surrounding the discs, while disc herniation occurs when nerves are compressed by the slipped disc.
Awareness of the fundamental differences between sciatica and intervertebral disc herniation is important for accurate diagnosis and appropriate treatment planning. Therefore, individuals experiencing back pain are advised to visit a specialist doctor to assess their condition, determine the probable cause of symptoms, and establish a comprehensive treatment plan.
Does walking help in treating cartilage?
Cartilage problems are among the most common diseases affecting the musculoskeletal system, and many people may suffer from cartilage pain and its resulting limited movement. Among the available treatments, whether medicinal or natural, walking is at the top of the list. In this article, we will explore the role of walking in treating cartilage and its potential benefits.
Improving Blood Circulation: Thanks to walking, blood circulation in the affected cartilage areas is improved, due to the increased blood flow to these vital areas. This provides the necessary oxygen and nutrients to nourish and regenerate the cartilage, enhancing the chances of restoring its health and vitality.
Strengthening Surrounding Muscles: Walking works to strengthen the muscles surrounding the cartilage, which helps to better distribute pressure on the joints and relieve excessive pressure on the damaged cartilage. This contributes to reducing pain and improving the cartilage’s ability to withstand stress.
Increasing Flexibility and Movement: Regular walking contributes to increasing the flexibility and range of motion of the joints, including those affected by cartilage problems. Developing joint flexibility improves overall movement and reduces issues of restrictions and stiffness.
Maintaining Optimal Weight: Maintaining an optimal weight is an important factor in the treatment and prevention of cartilage problems. Regular walking helps burn calories and maintain an ideal weight, which reduces the extra pressure on the cartilage and decreases the likelihood of problems occurring or worsening.
Improving Mood and Overall Well-being: Walking is a simple yet effective exercise for improving mood and increasing a sense of overall well-being. Walking releases happy chemicals in the brain such as endorphins and serotonin, which helps to alleviate pain and improve the overall state of individuals suffering from cartilage problems.
Can Cartilage Rebuild Itself?
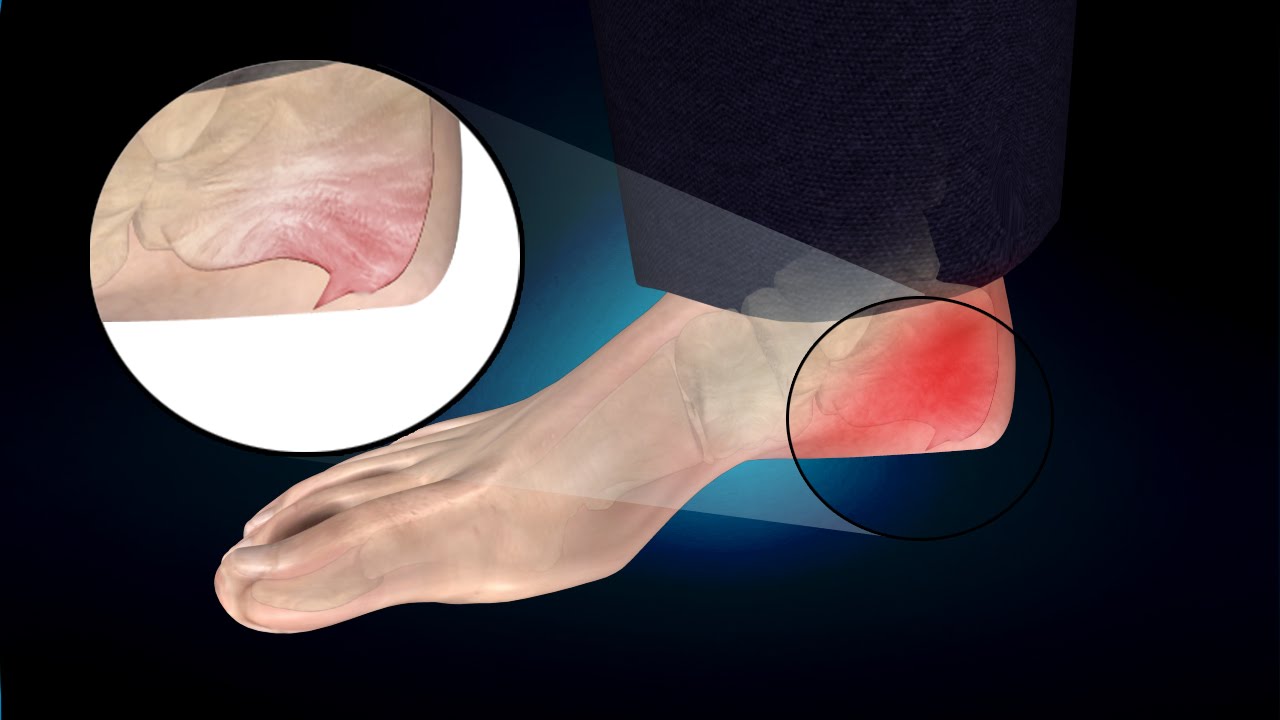
Cartilage is an important part of the human movement system, as it is found in the body’s joints and helps to reduce the force of friction and vibrations that occur during movement. However, cartilage does not have the ability to rebuild itself in the same ways that the body repairs its connective tissue after injury.
When cartilage is damaged, whether due to aging, continuous mechanical stress, or sports injuries, its ability to recover is limited. Cartilage is a collagen-rich tissue that lacks an active blood network and requires oxygen and nutrients delivered through the blood. Therefore, cartilage tends to suffer from poor healing ability.
However, there are some methods that can contribute to enhancing the flexibility of cartilage and boosting its recovery ability. For example, physical exercises and physiotherapy are used as part of rehabilitation to strengthen weak cartilage. Additionally, some dietary supplements containing important components such as glucosamine and chondroitin can be used to promote cartilage health.
Nevertheless, early awareness and prevention of harm are the most effective ways to maintain cartilage health. By regularly practicing physical exercises, avoiding risky sports injuries, and maintaining a healthy weight, the chances of cartilage damage can be reduced and its ability to recover in case of injury can be improved.
In general, although cartilage does not have the ability to fully rebuild itself, proper care of cartilage and following a healthy lifestyle can contribute to maintaining its health and reducing associated problems.
What are the degrees of disc herniation?
Disc herniation is one of the most common conditions in the spine, and it pertains to a change in the position of the intervertebral disc in the vertebrae. When herniation occurs, the disc moves away from its normal position, which may lead to irritation of the surrounding nerves, pain, and reduced flexibility of the spine. Disc herniation is common because the intervertebral discs are strongly affected by daily activities, stress, genetic factors, and aging.
There are several degrees of disc herniation, determined according to the severity of the change in the disc’s position and its impact on the spine. Below are the details of these degrees:
Mild Disc Herniation: In this case, the intervertebral disc has moved slightly from its normal position. Severe symptoms may not appear, and the pain may be mild and temporary. It is usually treated with rest and physical therapy. Moderate Disc Herniation: This refers to a condition where the intervertebral disc has moved further from its normal position. Disturbing symptoms and persistent pain in the affected area may appear. It usually requires intensive physical therapy and medications to relieve pain and inflammation. Severe Disc Herniation: Occurs when the intervertebral disc significantly shifts from its normal position. It can cause severe symptoms such as the inability to move and mobilize, numbness in the legs, and severe pain. It usually requires surgical treatment to restore the function of the spine and relieve pain.
If a disc herniation is suspected, it is advised to visit a specialist in the spine for an accurate diagnosis and appropriate treatment. Maintaining a healthy weight and regularly practicing physical exercises to strengthen the back muscles and reduce pressure on the spine may also be recommended.
Cartilage Procedure with Thermal Radiofrequency
The cartilage procedure with thermal radiofrequency is considered one of the innovative and effective methods to treat cartilage problems in the spine. This innovative procedure is offered by Dr. Amr Amal, a specialist in spine surgery and endoscopic surgical operations.
Cartilage diseases are one of the common health challenges faced by people around the world. These problems may arise due to aging, sports injuries, or even infections of the spine. The dysfunction in the cartilage leads to the emergence of distressing symptoms such as pain, numbness, and muscle weakness.
Dr. Amr Amal is distinguished by his extensive experience and high knowledge in the field of spine surgery, making him one of the best specialists in this domain. Using the thermal radiofrequency cartilage technique, Dr. Amal provides a safe and effective solution for people suffering from chronic cartilage issues.
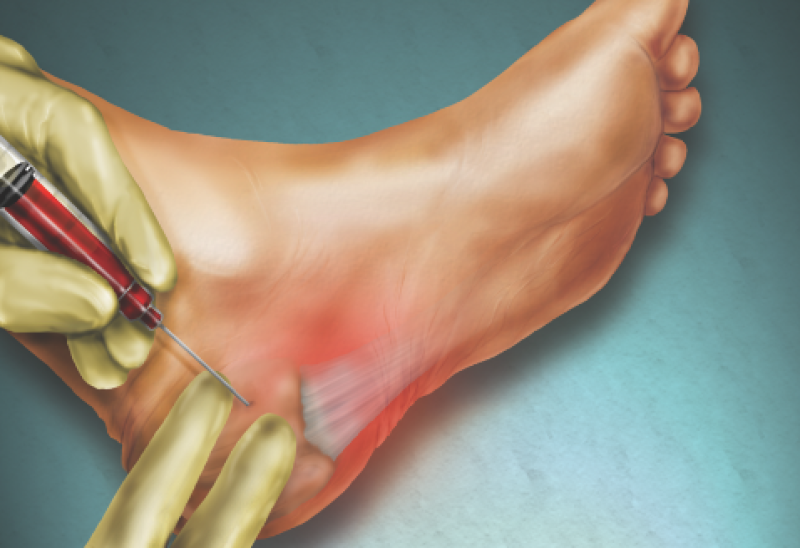
The cartilage procedure with thermal radiofrequency relies on regenerating the damaged tissue in the cartilage through stimulating cellular growth. This is achieved using a precisely controlled and regulated thermal radiofrequency technique. The device used in the procedure is attached to the spine for a specific period, where it applies concentrated heat to the affected area.
The cartilage procedure with thermal radiofrequency is a non-surgical operation, as it does not require any incisions or cuts in the skin. Thanks to this modern endoscopic approach, patients can benefit from a short recovery period and accurate diagnosis of cartilage problems in the spine.
In summary, the cartilage procedure with thermal radiofrequency is an important medical innovation in the field of spine surgery. It has proven effective in improving the conditions of patients suffering from chronic cartilage issues. Thanks to Dr. Amr Amal’s expertise and investment in this technique, patients can now return to a healthy and pain-free lifestyle.
In short, the cartilage procedure with thermal radiofrequency aims to improve cartilage health and alleviate distressing symptoms, enabling patients to live a better and more comfortable life under the care of Dr. Amr Amal, a leading expert in the field of spine surgery.