Herniated Disc in the Fifth Lumbar Vertebra: Causes and Treatment
أخر تحديث :
Herniated Disc in the Fifth Lumbar Vertebra
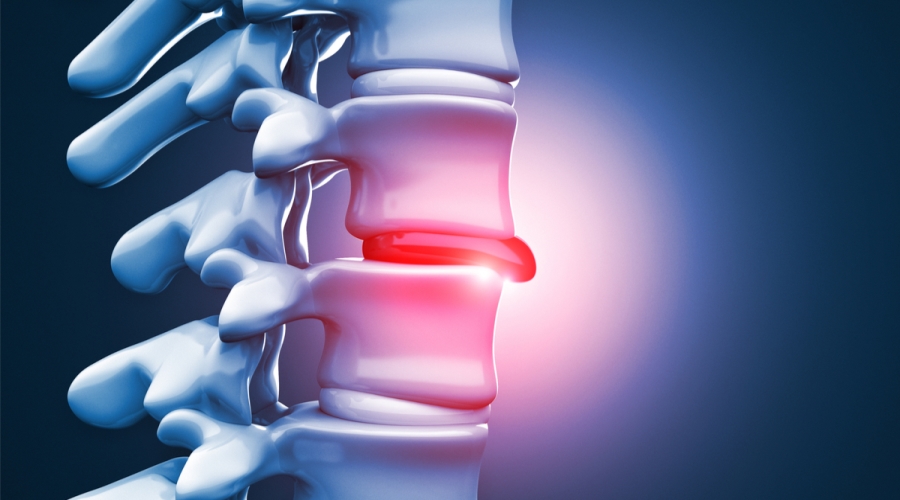
Herniated disc in the fifth lumbar (L5) vertebra is a common condition that occurs due to changes in the intervertebral disc as a result of aging. This type of herniated disc is prevalent among many individuals and can cause several painful and troublesome symptoms. The lack of fluids in the intervertebral disc between the vertebrae leads to herniation, resulting in the displacement of the spinal disc, which can cause forward movement of one of the vertebrae.
Several factors are responsible for the occurrence of herniated disc in the fifth lumbar vertebra. Among these factors are strenuous work that involves heavy lifting and repetitive movements of the spine. Obesity, smoking, prolonged sitting, and irregular exercise can also contribute to herniated discs.
The symptoms accompanying herniated disc in the fifth lumbar vertebra can range from pain, tingling, and weakness in the legs, buttocks, and feet. Patients may experience severe pain in the back, legs, hips, and buttocks, often accompanied by numbness and tingling in the legs and feet. Symptoms may worsen when walking or standing for extended periods and improve when sitting or lying down.
To treat herniated disc in the fifth lumbar vertebra, the patient should learn to manage the condition and follow medical guidance in their daily life. Patients are advised to avoid prolonged sitting and standing without breaks. Proper standing posture, such as military standing or raising one foot slightly, can help alleviate the pain and tingling caused by herniated discs. The exercise aims to open the nerve channel as much as possible, reducing the disc herniation in the spinal column.
The diagnosis of herniated disc in the fifth lumbar vertebra should be made by specialized doctors, and the appropriate treatment should be determined based on the patient’s condition. Treatment may include pain-relieving and anti-inflammatory medications, physical therapy, and specific exercises aimed at strengthening the muscles surrounding the spinal column, as well as preventive measures to avoid strenuous movements and reduce excess weight if present.
In general, herniated disc in the fifth lumbar vertebra is a common and treatable condition. Patients should adhere to medical guidance and adopt a healthy lifestyle to prevent worsening of symptoms and improve their quality of life. Treatment may require time and patience, but with the necessary care and treatment, patients can improve their condition and lead a normal and active life.
Can Herniated Disc Occur in the Lumbar Vertebrae?
Herniated disc is a common condition that affects the spinal column and can occur in any part of the spine, including the lumbar vertebrae. The lumbar vertebrae are the last five vertebrae in the spinal column and are an important region that bears a lot of pressure and movement.
Herniated disc occurs when the disc that separates the vertebrae and acts as a shock-absorbing cushion slips and causes pressure on the surrounding nerves. Herniated disc in the lumbar vertebrae can result from several factors, including:
- Insufficient fluids in the intervertebral disc: The intervertebral disc between the vertebrae typically contains a high percentage of fluids, which play a vital role in providing balance and support. When there is a decrease in these fluids, the risk of herniated disc increases.
- Tears in the outer layer of the intervertebral disc: Damage to the outer layer of the intervertebral disc can lead to fluid leakage inside it, reducing its ability to absorb shock and protect. This increases the likelihood of herniated disc.
- Limited movement and an inability to stand for extended periods: Excessive physical activity or lack of sufficient movement can lead to weakened back muscles and deterioration of the intervertebral disc, increasing the risk of herniated disc.
To cope with herniated disc in the lumbar vertebrae and alleviate accompanying symptoms, it is recommended to follow some medical advice in daily life, such as:
- Strengthening the back muscles and improving flexibility through appropriate exercises and core muscle-strengthening exercises.
- Maintaining proper body posture while sitting and standing, avoiding prolonged periods of sitting without movement.
- Avoiding heavy lifting and using proper lifting techniques.
- Paying attention to proper sleeping positions and using suitable pillows to support the spine.
- Maintaining a healthy weight and avoiding obesity, as excess weight can increase pressure on the vertebrae and the risk of herniated disc.
In the case of herniated disc in the lumbar vertebrae, the patient may be recommended to immobilize and rest for a specific period, and physical therapy may be advised to strengthen muscles and improve flexibility. In more severe cases, surgery may be necessary to repair the herniated disc and alleviate the accompanying symptoms.
In summary, herniated disc can occur in the lumbar vertebrae due to various factors, and it is essential to follow medical advice and adopt a healthy lifestyle to cope with this condition and reduce accompanying symptoms. Consulting a specialized doctor is necessary for diagnosis and determining the appropriate treatment.
When Does Herniated Disc Lead to Paralysis?
Herniated disc is a condition that occurs when the intervertebral disc, located between the vertebrae of the spinal column, shifts from its natural position. Herniated discs can occur in any part of the spine, but they are most common in the cervical (neck) and lumbar (lower back) vertebrae.
Herniated disc is a common condition and can result from aging, injury, or improper use of the spine. In rare and advanced cases, herniated disc can lead to paralysis when there is direct compression of the spinal cord.
When herniated disc occurs and the spinal cord is compressed, it can damage the nerve fibers responsible for movement and sensation in the body. Large and advanced herniated discs can lead to complete sensory loss in the area controlled by the compressed part of the spinal cord.
If the herniated disc is mild and does not cause significant nerve compression, non-surgical treatment may be sufficient. Treatment may include pain-relieving medications and physical therapy to strengthen the muscles around the spine and improve flexibility.
However, in cases of advanced herniated disc with significant nerve compression, surgical treatment may be the preferred option. Surgery involves removing the damaged part of the intervertebral disc and relieving the pressure on the affected nerves. It is important to diagnose and treat herniated disc early to avoid worsening symptoms and serious complications. Consultation with a neurosurgeon or spine specialist is necessary to evaluate the condition and determine the appropriate treatment.
In conclusion, recovery from herniated disc varies from person to person and depends on several factors, such as the size of the herniation, the duration of the injury, and the individual’s overall health. Symptoms may gradually improve over several weeks to months, but complete recovery may take longer in some cases.
It is essential to follow the treating physician’s instructions and adhere to the prescribed treatment for the best therapeutic results and to avoid worsening the condition. Complementary treatments such as physical therapy and appropriate exercises to strengthen the muscles and improve flexibility in the spine may also be beneficial.
Herniated Disc Diagnosis and Treatment:
Herniated disc should be diagnosed by a specialist, such as a spine surgeon. The doctor performs the necessary examinations and medical tests to identify sensitive areas and determine the cause of pain. Sometimes, additional tests like X-rays or magnetic resonance imaging (MRI) may be required to better assess the condition of the spine.
Generally, prevention of herniated discs involves maintaining a healthy weight and regular exercise. It is also advised to avoid prolonged sitting and practice safe driving. If you experience any symptoms similar to herniated disc, it is important to consult a doctor for an accurate diagnosis and appropriate treatment.
What Is the Treatment for Lumbar Disc Herniation?
Lumbar disc herniation occurs when the intervertebral disc between the lumbar vertebrae shifts from its natural position. This herniation can cause severe pain, numbness, tingling in the lower limbs, and reduce a person’s ability to move easily. Therefore, treating lumbar disc herniation is essential to alleviate symptoms and improve the quality of life.
The treatment methods for lumbar disc herniation depend on the degree of herniation and the severity of the symptoms. Medications, such as pain relievers and anti-inflammatories, may be used, and muscle relaxants may be prescribed if there is muscle spasm due to the herniation. Physical therapy is an important option for treating lumbar disc herniation, as it helps strengthen the back muscles and increase flexibility. Combining physical therapy with medications can be an effective solution, but not in all cases.
In severe cases of herniation and when previous treatments are not effective, surgery may be considered. The surgical procedure aims to stabilize the spine by permanently fusing the affected vertebrae, preventing movement between them. The decision to proceed with surgery is based on a thorough evaluation of the condition and the recommendations of the treating physician.
In addition to the mentioned treatments, other approaches may also be used in the treatment of lumbar disc herniation. Occasionally, spinal injections may be administered by injecting certain pain-relieving or anesthetic medications in the area surrounding the spinal cord. Physical therapy to strengthen the muscles and improve flexibility can also be beneficial.
It is important that lumbar disc herniation is diagnosed by a specialist and that the appropriate treatment is followed for the condition. Treatment may require a long period of time and patience to achieve noticeable improvement. Therefore, patients should adhere to the doctor’s instructions, attend prescribed therapy sessions, and follow up regularly.
In general, individuals suffering from lumbar disc herniation should adopt a healthy lifestyle that includes appropriate exercise, maintaining a healthy weight, and avoiding activities that increase pressure on the spine. It is also recommended to avoid strenuous positions and strengthen the neck and back muscles as a preventive measure against herniation.
Does Massage Help with Herniated Disc?
Massage is a therapeutic technique used to alleviate muscle tension, spasms, and improve blood circulation in the body. Numerous studies have shown that massage can be effective in treating various medical conditions, including herniated discs.
Herniated disc is a condition that occurs when the intervertebral disc between the vertebrae moves out of its natural position. It can cause severe pain, numbness, tingling, and weakness in the limbs. For people with herniated discs, massage can be an effective method for reducing pain and improving their condition.
A study conducted at Indiana University in the United States found that localized massage can be an effective treatment for lower back pain associated with herniated discs. Researchers evaluated the impact of massage on a group of patients experiencing back pain and found that localized massage could reduce pain and improve the quality of life for these patients.
Massage sessions work by stimulating the tissues and muscles around the affected area. By increasing blood flow to the area, massage can help reduce swelling and improve the healing process of damaged tissues. It can also increase muscle flexibility and aid in restoring the natural range of motion. However, it’s essential that massage is performed by a qualified and specialized therapist. Incorrect massage techniques can exacerbate symptoms and lead to additional issues. Therefore, treatment should be guided by a physical therapist or manual therapist.
There are different types of massage that can help in the treatment of herniated discs. For example, Swedish massage uses gentle to moderate pressure movements to stimulate blood circulation and relieve muscle tension. Deep tissue massage, on the other hand, uses deeper pressure to focus on deep muscles and alleviate deep muscle tension.
In addition to massage, rest and avoiding strenuous activities should be considered to prevent excessive strain on the spine. Rest can be beneficial in cases of mild herniated discs, as the body can naturally recover without the need for surgical intervention. In general, massage can be helpful in treating herniated discs if performed correctly and under medical supervision. However, it is essential to consult a doctor before starting any treatment to ensure it is suitable for the patient’s condition and does not conflict with any other treatments they may be receiving.
What Is the Difference Between Cervical and Lumbar Vertebrae?
Cervical and lumbar vertebrae are both part of the spine and each has its unique characteristics. Cervical vertebrae are the vertebrae located below the neck, between the thoracic and lumbar vertebrae. Cervical vertebrae are larger and thicker compared to thoracic and cervical vertebrae, primarily because they bear a more significant portion of the body’s weight. They are the second-largest vertebrae in terms of size after lumbar vertebrae.
Cervical vertebrae consist of seven vertebrae and are located between the thoracic and cervical regions of the spine. These vertebrae are characterized by kidney-shaped bodies and short, thick plates and are composed of five bone pieces that articulate with each other through the intervertebral disc. Cervical vertebrae are more prone to pain, possibly due to the extra stress they bear as a result of supporting a more substantial portion of the body’s weight.
Lumbar vertebrae, on the other hand, are the vertebrae located in the lower part of the spine, and they consist of five vertebrae. Lumbar vertebrae are thicker and larger than cervical vertebrae and are responsible for bearing most of the body’s weight. Lumbar vertebrae are directed inward, forming a lordotic curve in the spine. These vertebrae become ossified and fused as individuals reach adulthood.
Cervical and lumbar vertebrae differ in several aspects. Cervical vertebrae are larger and thicker, bearing a significant portion of the body’s weight. Lumbar vertebrae, while also located in the lumbar region, carry most of the body’s weight.
In general, it can be said that the difference between cervical and lumbar vertebrae lies in their location in the spine, their size, and their role in bearing weight. Cervical vertebrae are located between the thoracic and lumbar vertebrae and bear the larger portion of the body’s weight, while lumbar vertebrae are located in the lower part of the spine and also bear most of the body’s weight.
Regardless of the differences between cervical and lumbar vertebrae, it is essential to care for the health of the spine in general. It is recommended to engage in appropriate physical exercises and maintain good posture while sitting and standing to preserve spinal health, reduce pain, and prevent potential issues in the future.
Does Lumbar Herniated Disc Affect the Knee?
A lumbar herniated disc is a condition that occurs when the intervertebral discs between the vertebrae that make up the spinal column in the lower back are compressed. Can a lumbar herniated disc affect the knee?
Firstly, it is important to note that a lumbar herniated disc primarily affects the nerves emanating from the spinal column and does not directly impact the knee. However, a lumbar herniated disc can lead to a feeling of instability in the knee or an inability to move it as usual, accompanied by continuous knee pain.
When a lumbar herniated disc occurs, it can result in increased pressure on the nerves branching from the spinal column and extending to the knee. This increased pressure on the nerves may lead to knee pain and a sense of instability or an inability to move it normally.
Additionally, the affected knee joint may become more susceptible to developing osteoarthritis. Osteoarthritis is a condition that causes joint damage and leads to chronic pain and reduced mobility. Since the knee is one of the major joints in the body, a lumbar herniated disc can potentially increase the likelihood of developing osteoarthritis in the affected knee.
It is worth mentioning that knee pain and stiffness are not necessarily directly related to a lumbar herniated disc. You may have increased ligament laxity, which can cause knee pain. Therefore, it is essential to consult a doctor to determine the true cause of the symptoms you are experiencing.
To treat a lumbar herniated disc in the lower back and alleviate knee pain, some measures can be taken. Ice packs can be applied to the lower back area to reduce inflammation and relieve pain. Additionally, cupping therapy can be an effective natural option for pain relief and improving blood circulation in the affected area.
In conclusion, it can be said that a lumbar herniated disc can indirectly affect the knee by increasing pressure on nerves and potentially increasing the risk of developing osteoarthritis in the knee. If you are experiencing knee pain or symptoms suggestive of a lumbar herniated disc, it is essential to consult a doctor for a diagnosis and appropriate treatment.
The Best Spinal Fixation Doctor in Egypt
Dr. Amr Amal is one of the top spinal fixation doctors in Egypt. Dr. Amr Amal is renowned as one of the leading orthopedic consultants in Egypt and possesses extensive expertise in spinal surgery and orthopedics.
Dr. Amr Amal graduated as an orthopedic physician from Ain Shams University Medical School with honors. He worked as a resident physician at Ain Shams University Hospitals for three years and as an assistant lecturer at Ain Shams University Hospitals for five years. He currently serves as a lecturer in orthopedic, joint, and arthroscopic surgeries at Ain Shams University.
Dr. Amr Amal is distinguished by multiple specialties and extensive experience in the field of spinal surgery and orthopedics. He offers comprehensive and effective treatment for spinal issues and acute injuries using advanced techniques such as plates and screws. Dr. Amr Amal and his specialized spinal fixation team aim to restore spinal mobility and improve patients’ daily quality of life. They provide holistic care, efficiently diagnosing and treating bone problems.
Thanks to his vast experience and high specialization, Dr. Amr Amal is considered one of the best doctors in the field of spinal fixation in Egypt. He utilizes the latest medical techniques and tools to achieve the best results for patients. If you are experiencing bone issues or require spinal fixation surgery, Dr. Amr Amal is the optimal choice for you. You can contact him and schedule an appointment to receive the appropriate treatment for your condition.
By choosing Dr. Amr Amal, you will receive comprehensive care and effective treatment for bone problems and spinal fixation in Egypt.