Learn about Hidradenitis Suppurativa and what causes it
Hidradenitis Suppurativa
Many individuals suffer from a chronic condition known as Hidradenitis Suppurativa, which extends from the lower back to the feet. In this article, we will cover several points to understand this condition and how to deal with it:
Common Symptoms of Hidradenitis Suppurativa Possible Causes Treatment and Self-Care Surgical Procedures Prevention
In general, Hidradenitis Suppurativa can be managed through the use of pain relievers, anti-inflammatories, proper rest, and appropriate physical activity, while avoiding improper movements. If the pain continues to worsen or significantly affects your mobility, it’s advisable to consult a doctor for an assessment and an appropriate treatment plan.
What Are the Symptoms of Hidradenitis Suppurativa and How Is It Treated?
Hidradenitis Suppurativa is a neurological disorder that affects the sciatic nerve, and it can cause distressing and painful symptoms for patients. Here, we provide you with information on how to recognize if you have Hidradenitis Suppurativa and some available treatment options:
- Severe Pain: The pain in cases of Hidradenitis Suppurativa is extremely severe and can only be described as excruciating. A person may feel this pain from the lower back to the toe, and it may worsen with movement or prolonged sitting.
- Tingling and Numbness: Individuals with Hidradenitis Suppurativa may experience tingling and numbness in their legs. This sensation can be constant or intermittent and usually occurs in the thighs or legs.
- Reduced Mobility: Hidradenitis Suppurativa can significantly affect a person’s ability to move. They may have difficulty standing for extended periods or walking normally, and they may feel weakness in their legs.
- Changes in Sexual Function: Those with Hidradenitis Suppurativa may notice changes in their sexual function, such as difficulty with erections or reduced sexual desire. These changes may result from pressure on the nerves responsible for sexual organ function.
- Psychological Impact: Hidradenitis Suppurativa can impact the individual’s mental well-being. They may experience anxiety, depression, and irritability due to constant pain and the limitations it imposes on their daily life.
The treatment methods for Hidradenitis Suppurativa depend on the severity of the symptoms and the medical diagnosis. Here are some available options for treating Hidradenitis Suppurativa:
Natural Treatment: Physical therapy includes muscle strengthening exercises, improving flexibility, and balance. This option can be beneficial in relieving pain and enhancing mobility.
Medication Treatment: A doctor may recommend taking pain relieving and anti-inflammatory medications to alleviate pain and reduce inflammation. Consultation with a doctor regarding the dosage and suitability of these medications is necessary.
Interventional Treatment: This type of treatment involves the use of techniques such as therapeutic massage, heat therapy (such as heating or cooling), and psychological training to reduce pain and increase comfort.
Surgical Treatment: In severe cases where patients do not respond to other treatments, the doctor may recommend surgery to relieve pressure on the affected nerve.
Consulting with a physician is essential for diagnosing and treating Hidradenitis Suppurativa correctly. Treatment should align with individual needs and the severity of the symptoms. Ultimately, remember that walking and engaging in light physical activity may be helpful in relieving pain and promoting recovery.
Can Hidradenitis Suppurativa Be Cured?
Hidradenitis Suppurativa is a common condition experienced by many, but can it be cured? Let’s find out:
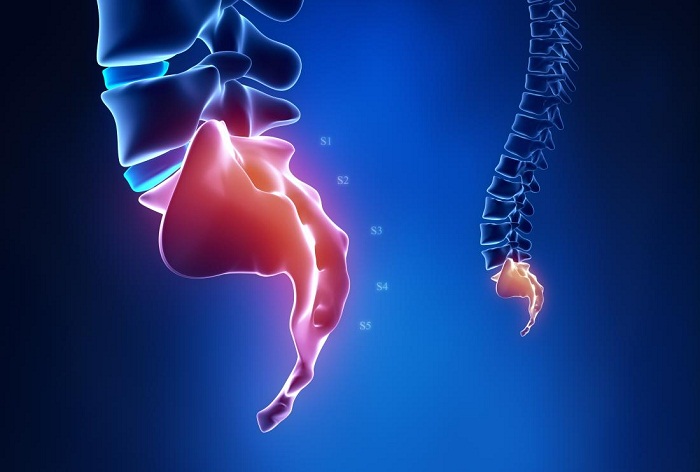
Understanding Hidradenitis Suppurativa: Hidradenitis Suppurativa is a condition characterized by pain in the muscles and nerves in the lower back and legs. The pain can be continuous or intermittent and may be accompanied by tingling and numbness. Research suggests that Hidradenitis Suppurativa occurs due to pressure on the nerves in the spinal column, either due to spinal disc narrowing or herniation.
Self-Care: For most people, Hidradenitis Suppurativa responds to self-care measures. Applying cold compresses to the affected area and avoiding excessive activity that can exacerbate symptoms is recommended. Rest is necessary to alleviate pain, but it’s essential to work on regaining movement and performing necessary exercises to strengthen muscles and improve flexibility.
Medical Treatment: In some cases, the pain can be extremely severe and unmanageable with self-care measures alone. In these instances, a person may require specialized medical treatment. A doctor may prescribe pain-relieving medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), and sometimes local nerve blocks and stimulants.
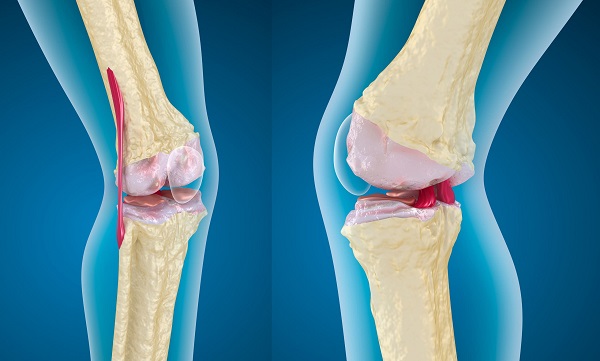
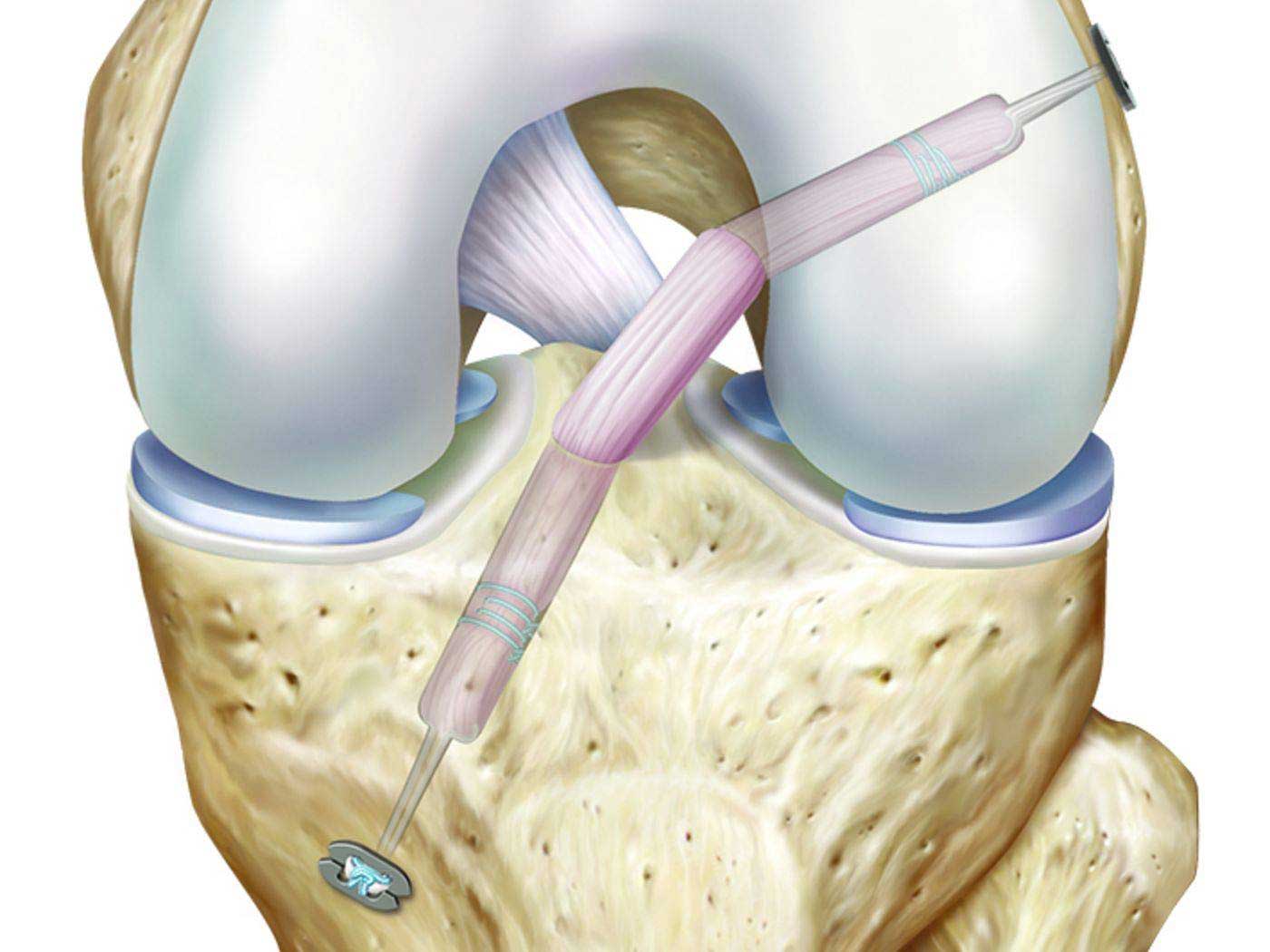
Surgical Treatment: In extremely rare cases, the pain and symptoms of Hidradenitis Suppurativa may remain uncontrollable even after trying all other treatments. In these situations, surgery may be an option. Surgical procedures may involve removing bone spurs or a portion of the herniated disc compressing the nerve. Surgeons typically perform this surgery when a person experiences severe weakness or a significant decline in organ function or chronic pain.
Although Hidradenitis Suppurativa can be a challenging and painful condition for many individuals, most cases can significantly improve with appropriate self-care and medical attention. If you are experiencing symptoms of Hidradenitis Suppurativa, it is advisable to consult a specialized physician for an evaluation and guidance towards the appropriate treatment.
How is Hidradenitis Suppurativa Treated?
Hidradenitis Suppurativa is a common condition that causes numbness and severe pain in the lower back area due to the herniation of spinal discs. This condition may require prompt and effective treatment to alleviate pain and improve mobility. Here is a list of the top 10 methods that can be used to treat Hidradenitis Suppurativa:
- Home Treatment and Exercises: Patients can perform simple home exercises that help strengthen muscles and improve spinal stability. These exercises include hamstring stretches, knee-to-chest stretches, lateral stretches, and more.
- Medications: Doctors may prescribe pain-relieving and non-steroidal anti-inflammatory drugs (NSAIDs) to alleviate pain and inflammation in the Hidradenitis Suppurativa area.
- Massage: Massage therapy can help relieve muscle tension and improve blood flow to the affected area of Hidradenitis Suppurativa.
- Cupping Therapy: Cupping therapy, a treatment technique involving the placement of transparent cups on the body to create suction and stimulate blood flow, is believed to contribute to pain relief and enhance spinal function.
- Surgery: In cases where the condition does not respond to non-surgical treatments, surgery may be recommended to remove or stabilize the affected herniated disc and reduce pressure on the nerves.
- Hot and Cold Compresses: Hot and cold compresses can be used to alleviate pain and vary muscle tension. Cold compresses are preferred in the early stages of the injury, while hot compresses can be used later to increase blood flow and accelerate tissue healing.
- Local Anesthesia: In cases of severe pain, doctors may inject local anesthetics into the affected part of the spine to numb the area and relieve pain.
- Traction: In some severe cases resistant to other treatments, traction may be recommended as a method to alleviate pain and improve the condition of patients with Hidradenitis Suppurativa.
- Physical Therapy: Physical therapy exercises and sessions can help improve flexibility, muscle stability, and alleviate pain associated with Hidradenitis Suppurativa.
- Proper Posture: It is recommended to maintain proper posture when sitting, standing, and lifting heavy objects to prevent worsening Hidradenitis Suppurativa and reduce pressure on the spine.
To maximize the benefits of these methods, it is advisable to consult a specialized physician for a proper diagnosis and determine the most suitable treatment based on individual patient details and the severity of the condition.
What Are the Causes of Sciatica?
Sciatica pain is a common health issue that affects many individuals. Sciatica can occur due to several different reasons, and understanding these causes can help improve health awareness and determine appropriate care. Here are some common causes of sciatica:
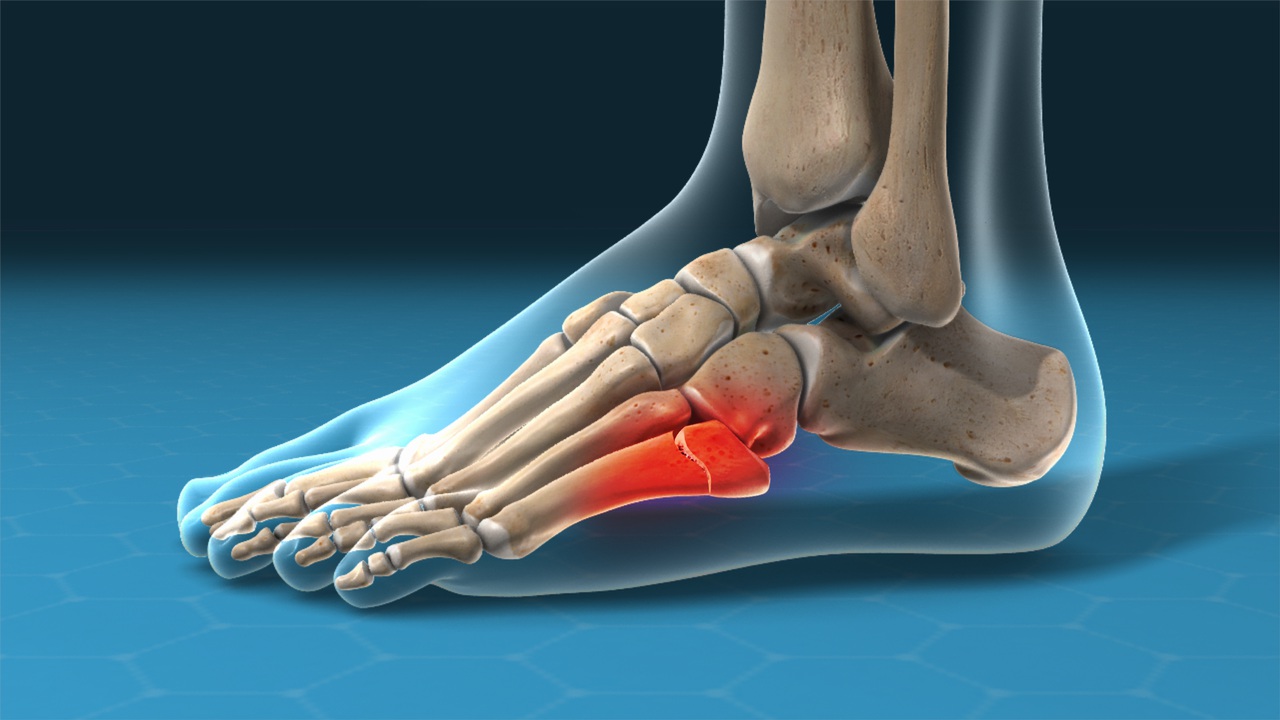
- Herniated Disc: A herniated disc is a very common cause of sciatica. When a spinal disc slips or herniates, it can affect the nerve roots and cause compression, leading to sciatica pain.
- Disc Degeneration: Degeneration of the spinal discs can also lead to sciatica. As discs wear down and lose their cushioning ability, they can place pressure on nerve roots.
- Piriformis Syndrome: The piriformis muscle, located in the buttocks, can sometimes irritate or compress the sciatic nerve, resulting in sciatica symptoms.
- Spinal Stenosis: Spinal stenosis, the narrowing of the spinal canal, can lead to pressure on the nerve roots and cause sciatica pain.
- Spondylolisthesis: This condition occurs when one vertebra slips forward over another, potentially compressing the nerve roots and causing sciatica.
- Trauma: Injuries to the spine, such as fractures or dislocations, can lead to sciatica if they impact the nerve roots.
- Tumors: Rarely, tumors or growths in the spinal canal can press on nerve roots and result in sciatica.
- Infections: Infections affecting the spine or the tissues surrounding it can lead to sciatica symptoms.
- Obesity: Excess body weight can increase the risk of sciatica as it places additional stress on the spine and nerve roots.
- Other Factors: There can be other less common or specific factors contributing to sciatica, such as spinal cord abnormalities or certain medical conditions.
Many factors can increase the risk of developing sciatica, including age and underlying health conditions. It is essential to consult a doctor to determine potential causes and appropriate treatment options.
In conclusion, if you are experiencing sciatica pain, it is advisable to visit a healthcare provider for an accurate diagnosis and a tailored treatment plan. Remember that each case is unique and deserves individual attention.
Treatment for Sciatica in Men:
The appropriate treatment for sciatica is determined based on the severity of the symptoms and their impact on daily life. Treatment may include the use of pain-relieving medications, strengthening the muscles surrounding the affected nerve, physical therapy, and lifestyle changes.
Tips for Preventing Sciatica:
It is important to engage in regular physical exercises with warm-up and stretching routines to strengthen muscles and improve flexibility.
Maintaining a healthy weight and consuming a balanced diet can contribute to preventing nerve-related issues.
In summary, sciatica in men can affect either the right or left side. It is essential to diagnose and treat this condition by specialized healthcare providers to alleviate symptoms and enhance the quality of life.
Does Walking Affect Sciatica?
If you are experiencing sciatica pain and wondering if walking will affect your condition, you’ve come to the right place. In this article, we will explore the impact of walking on sciatica and the correct way to engage in it.
Benefits of Walking for Sciatica: Proper walking can help reduce the pressure on the muscles in the spine and the sciatic nerve. Sciatica refers to a specific type of sciatic nerve inflammation, which is one of the longest and widest nerves in the body. According to a study of 35,000 individuals, walking and cycling reduce the risk of developing sciatica by 33%.
Sciatica Pain While Walking: Sciatica pain can occur while walking, with the pain typically starting in the lower back and extending along the nerve’s path. To understand why pain might increase while walking, consider factors such as walking posture and technique. Some walking postures and techniques can increase pressure on the sciatic nerve, leading to heightened pain.
Relieving Sciatica Pain While Walking: To alleviate sciatica pain while walking, it is advisable to follow some tips. It may be best to adjust your walking posture and avoid positions that exert excessive pressure on the sciatic nerve. Standing with a straight back and focusing on proper walking form may help reduce sciatica pain.
Remember that before starting any new physical activity, it is always important to consult your healthcare provider for necessary guidance and to evaluate your health condition.
In conclusion, walking can be an effective treatment for sciatica if done correctly. Choosing the right posture and paying attention to proper walking techniques may help alleviate pain and improve the overall condition of sciatica patients.
Is Sciatica Surgery Dangerous?
Sciatica is a painful condition that causes severe pain in the lower limbs. While surgical procedures are rarely used to treat sciatica, some people may wonder about the safety of such surgery.
Here are some points to help answer this question:
High Success Rate: Sciatica surgery is typically considered safe and has a high success rate. Success depends on a precise diagnosis and assessment of the condition by a specialized physician.
Limited Risks: Sciatica surgery is not generally considered dangerous. However, patients may be exposed to some potential complications such as minor bleeding or infections in the affected areas.
Choosing a Skilled Surgeon: Selecting a skilled and experienced surgeon for sciatica surgery is essential to ensure success and avoid potential complications. Make sure to choose a reputable, board-certified surgeon.
Exploring Non-Surgical Options: Before suggesting surgery, non-surgical treatments are usually tried to alleviate pain and improve the patient’s condition. Natural treatments like physical therapy and exercise may be sufficient to improve the condition and reduce pain.
In conclusion, sciatica surgery is not dangerous when performed by a skilled surgeon and when the condition is accurately assessed. Before considering surgery, it is advisable to attempt non-surgical treatments and consult a physician to determine the optimal option for pain relief and overall improvement.
Is a Back Brace Helpful for Sciatica?
Back pain and sciatica are common problems for many people worldwide. To alleviate these pains, some individuals turn to the use of a back brace. But is a back brace really helpful for treating sciatica? In this article, we’ll provide some information on the effectiveness of back braces in relieving sciatica pain.
Pain Relief: A back brace offers effective support in relieving pain from conditions like herniated discs, sciatica, scoliosis, and spinal issues. This is due to its flexible and adjustable design, which helps stabilize the spine, reducing pressure on affected nerves and tissues.
Additional Support: Back braces come with sturdy lower support belts. These belts can be adjusted to suit individual needs, ensuring proper back support and improved posture. This additional support can be beneficial when regular comfort and relief are insufficient.
Daily Use: A back brace can be worn throughout the day, even during daily activities. It helps stabilize the spine and reduces pain caused by movement and exertion. This continuous usage can be helpful for individuals experiencing recurrent sciatica pain, as they can benefit from ongoing support without the need to remove or readjust the brace.
For Demanding Activities: A back brace provides the necessary support when a person needs to engage in activities that require physical effort, such as gardening or exercise. Individuals can turn to a back brace during these moments to ensure added support and reduce strain and pain.
However, some considerations should be kept in mind when using a back brace. Not all cases of sciatica respond well to brace usage, especially when there is pressure on the nerve roots. It is advisable to consult a physician before using a brace, particularly in cases of severe or persistent pain.
A back brace can be effective in relieving sciatica pain, but it is not the ultimate solution. It is recommended to use it as part of a comprehensive treatment plan that includes appropriate physical exercises and overall healthcare. Individuals should prioritize comfort and follow medical advice before using any type of back brace.
What Is Pseudosciatica?
Pseudosciatica, also known as Piriformis Syndrome or Hip Pseudo-sciatica, is a medical condition that occurs when the sciatic nerve is compressed in the surrounding areas, causing pain and symptoms that resemble true sciatica.
Pseudosciatica more commonly affects women and can develop suddenly after an accident or gradually over several months.
Symptoms of pseudosciatica may include:
- Pain in the hip, buttocks, and legs, which can radiate down to the foot.
- Tingling and numbness in the lower extremities.
- Increased pain when moving or sitting for extended periods.
- Weakness in leg muscles.
Diagnosing pseudosciatica requires examination and evaluation by a physician. This may include physical symptom assessment, magnetic resonance neurography (MRN), and FAIR testing.
While there is debate among researchers regarding the diagnosis of this condition, the necessary treatment varies from case to case and depends on several factors, including the duration and severity of the condition.
Potential treatments may include:
- Physical Therapy: Strength-building exercises for the muscles surrounding the sciatic nerve, stretching exercises, and muscle tension reduction.
- Medication: A doctor may prescribe pain-relieving medications or muscle relaxants to alleviate symptoms.
- Local Injections: In severe cases, a physician may administer a local injection, such as cortisone, to reduce inflammation and pain.
In general, pseudosciatica is not a chronic health problem and can be successfully treated in most cases. If you are experiencing symptoms similar to those described, consult a physician for a diagnosis and the appropriate treatment.
Does Sciatica Affect the Knee?
Sciatica is a condition where there is pressure on the sciatic nerves, which extend from the spine to the legs and terminate just below the knee. Consequently, sciatica can affect the knee and cause pain in this area.
In this list, we will explain the potential effects of sciatica on the knee and provide some tips on how to manage this condition:
- Knee Pain: Sciatica can cause sharp pain in the knee area. Affected individuals may experience tingling or a warm sensation in this region, or even sharp pain.
- Pain Radiating from the Back: Since sciatica often originates from spinal issues, it can extend to other parts of the body and cause problems. For instance, if there is pressure on the sciatic nerves from the spine, it can cause knee pain.
- Walking Difficulties: People with sciatica may experience abnormal walking patterns, leading to increased pressure on the knee and causing pain. Therefore, it is recommended to engage in exercises that strengthen the muscles surrounding the knee and thighs to maintain stability.
- Leg Weakness: In some cases, sciatica can lead to weakness in the affected leg or foot. This may make movement and walking difficult and increase the risk of falls.
- Bladder Control Issues: In rare cases, if there is severe pressure on the sciatic nerves in the spine due to sciatica, it can lead to loss of bladder control. If you experience this problem, it is important to consult a physician to assess the situation and provide appropriate treatment.
It is essential to pay attention to spinal health and follow the necessary guidelines to maintain a healthy back and alleviate sciatica pain. If you are experiencing knee pain or suspect the progression of your condition, it is advisable to visit a spine specialist or rehabilitation specialist to evaluate your condition and develop an appropriate treatment plan.
These are general information and do not substitute for consultation with a qualified healthcare professional. Always seek the guidance of a qualified healthcare provider for a diagnosis and suitable treatment for your condition.