Learn about the Symptoms of Lumbar Disc Herniation and Can it be Recovered from?

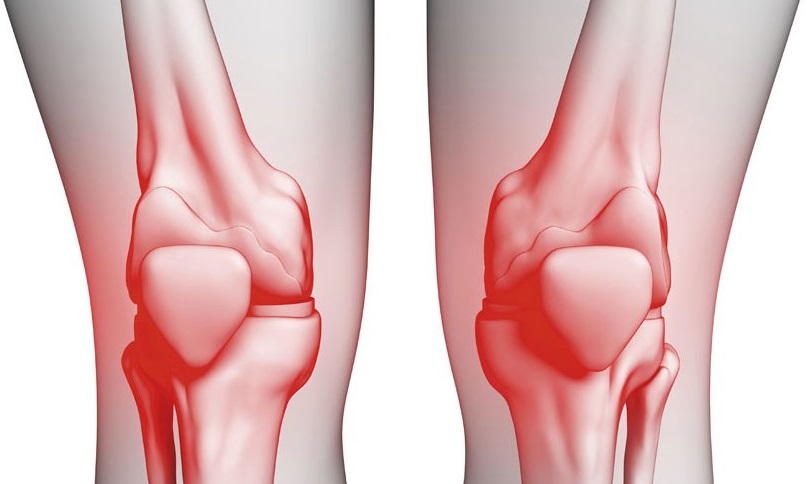
Symptoms of Lumbar Disc Herniation
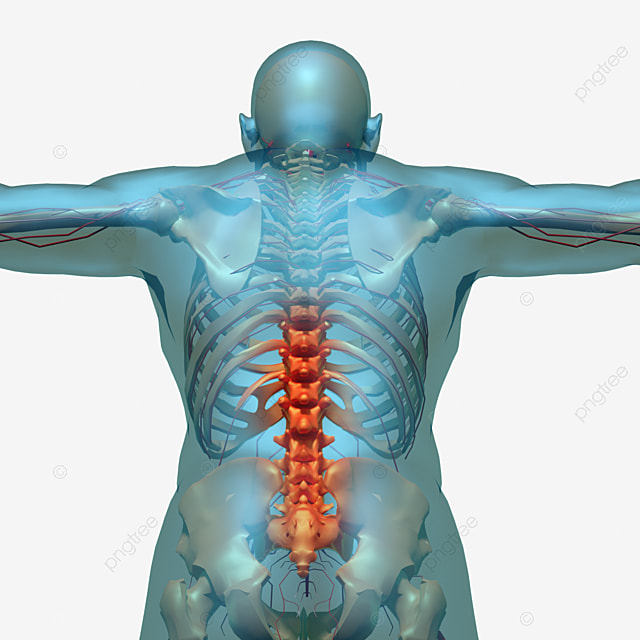
Lumbar disc herniation, also known as disc protrusion or disc herniation, is a medical condition that affects the spinal column. This term refers to the slipping or herniation of the spinal discs, which act as shock absorbers between the vertebrae in the spinal column. When these discs slip out of their normal position, they can cause painful symptoms and have negative effects on the affected person’s quality of life. In this article, we will detail the symptoms of lumbar disc herniation.
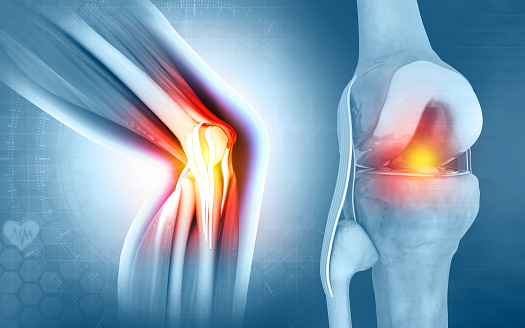
Key Symptoms of Lumbar Disc Herniation: Back Pain: Back pain is one of the most common symptoms for individuals suffering from lumbar disc herniation. This pain can be either acute or chronic and typically worsens when engaging in activities that put pressure on the spinal column. Leg Pain: Pain from the back can radiate down to the legs, a condition known as radicular leg pain. This pain can be severe and may occur alongside or separately from back pain. Muscle Weakness: Lumbar disc herniation can lead to weakness in the muscles associated with the affected area due to pressure on the nerves surrounding the herniated disc. Numbness and Tingling: Nerve compression can result in various sensory symptoms such as numbness and tingling in the legs. Changes in Bowel and Bladder Function: In rare cases, lumbar disc herniation can cause changes in bowel and bladder function due to pressure on the nerves responsible for these functions.
Can it be Recovered from?
The recovery from lumbar disc herniation varies depending on the severity of the condition and the individual’s response to treatment. Many people with mild to moderate lumbar disc herniation can experience significant improvement and even full recovery with conservative treatments such as physical therapy, pain medications, and lifestyle modifications.
In more severe cases or when conservative treatments do not provide relief, surgical intervention may be necessary. Surgical options include discectomy, laminectomy, and spinal fusion. Recovery from surgery may also vary, but with proper post-operative care and rehabilitation, many individuals can regain their mobility and function.
It’s important to note that early diagnosis and prompt treatment can play a crucial role in the recovery process. Therefore, if you experience any symptoms of lumbar disc herniation, it is advisable to consult with a healthcare professional for a proper evaluation and treatment plan tailored to your condition.
Prevention:
Lumbar disc herniation cannot always be completely avoided, but some preventive measures can help reduce the risk of injury, such as:
Maintaining a healthy weight. Regularly engaging in physical exercises to strengthen the back muscles. Maintaining good posture while sitting and lifting heavy objects. Avoiding activities that place excessive pressure on the spine.
In conclusion, the symptoms of lumbar disc herniation should be taken seriously, and appropriate medical care should be sought. Quick diagnosis and effective treatment can help alleviate pain and improve the quality of life for the affected individual.
Can Lumbar Disc Herniation Be Recovered From?
The recovery from lumbar disc herniation depends on several factors, including:
The Severity of Herniation: If the disc herniation is mild and does not exert significant pressure on the nerves or surrounding tissues, the chances of recovery are higher. In such cases, physical therapy and medications may be sufficient for improvement.
Location of Herniation: Recovery also depends on the location of the herniation in the spine. Some locations may be more complicated than others, and surgery may be necessary in some cases.
Treatment Response: The individual’s response to treatment plays a significant role in recovery. If the person follows the doctor’s advice, engages in physical exercises, and takes medications regularly, it increases the chances of recovery.
Overall, while recovery from lumbar disc herniation is possible, it depends on various factors. Early diagnosis and appropriate treatment can improve the chances of a successful recovery.
Treatment Methods:
Physical Therapy: This includes physical exercises and strengthening the muscles around the spine. Physical therapy can be effective in improving strength, flexibility, and pain reduction.
Medications: Anti-inflammatory drugs and pain relievers are used to alleviate pain and inflammation.
Epidural Injections: Cortisone or Botox injections can be helpful for some individuals in reducing pain.
Surgery: In severe cases and when there is little improvement after an extended period of treatment, surgery may be necessary to remove the herniated disc or repair tissue tears.
In conclusion, individuals with lumbar disc herniation can significantly improve their condition through appropriate treatment and following preventive measures. However, those with this condition should be prepared for long-term management and should reduce activities that may put additional pressure on the spine. If symptoms persist or worsen, individuals should consult their healthcare provider for further evaluation and treatment recommendations.
Can Lumbar Disc Herniation Cause Paralysis?
Lumbar disc herniation is a condition that affects the spine and the spinal discs located between the vertebrae. This condition is a source of concern for many, and one of the common questions from patients is whether lumbar disc herniation can lead to paralysis. In this article, we will discuss whether lumbar disc herniation can cause paralysis and how to manage this condition.
Lumbar Disc Herniation: Definition and Causes:
Lumbar disc herniation occurs when the disc that acts as a shock absorber between the vertebrae slips out of its normal position. This condition often results from the degeneration of spinal discs over time or due to injury or pressure on the spine. Lumbar disc herniation can be painful and lead to movement problems and discomfort.
Can Lumbar Disc Herniation Cause Paralysis?
Yes, lumbar disc herniation can cause paralysis in rare cases and when there is significant pressure on the spinal cord or nerve roots in the spine. Paralysis is the loss of the ability to control movement or sensation in a part of the body and can be partial or complete, depending on the location and severity of nerve compression.
Symptoms that may indicate significant nerve compression include:
Loss of sensation in a specific part of the body. Muscle weakness. Difficulty controlling movement.
In conclusion, while lumbar disc herniation can be painful and troublesome, it does not commonly lead to paralysis. If you are experiencing symptoms indicating significant nerve compression, seek immediate medical care for evaluation and appropriate treatment. Early diagnosis and effective treatment can reduce the risk of paralysis and improve treatment outcomes.
What’s the Difference Between Herniated Disc and Sciatica?
Herniated disc and sciatica are two common disorders that can cause pain and swelling in the back and spine area. While they share many symptoms, they differ in their causes, diagnosis, and treatment options. In this article, we will compare herniated disc and sciatica in terms of causes, symptoms, and treatment options.
Herniated Disc:
Causes: A herniated disc occurs when a disc of cartilage between the vertebrae slips out of its normal position. This movement often results from the degeneration of spinal discs over time or due to an injury. This herniation can put pressure on the spinal cord and the surrounding nerve roots, leading to pain, numbness, and weakness in the limbs.
Symptoms:
Back and neck pain. Pain radiating down the legs or arms, known as radicular leg or arm pain. Numbness or tingling in the affected area of the body. Weakness in the muscles associated with the affected area.
Treatment Options:
Physical therapy and rehabilitation exercises. Anti-inflammatory medications and pain relievers. Epidural injections to relieve pain and inflammation. In severe cases, surgery may be required to remove the herniated disc or repair tears.
Sciatica:
Causes: Sciatica is not a condition itself but a symptom of an underlying issue, often related to herniated discs or spinal stenosis. It occurs when the sciatic nerve, which runs from the lower back down the legs, becomes compressed or irritated. This compression can result from herniated discs, bone spurs, or spinal stenosis.
How long does herniated disc pain last?
The duration of herniated disc pain varies depending on several factors, including the severity of the herniation and the individual’s characteristics. Pain can persist for a temporary or chronic period in some cases. In this article, we will delve into the duration of pain in herniated disc cases and the factors that influence its duration.
Duration of pain in herniated disc cases:
- Severity of herniation: The severity of a herniated disc varies from one case to another. If the herniation is mild and does not exert significant pressure on nerves or surrounding tissues, the pain may be temporary and short-lived. In many cases, the pain can spontaneously subside over time with rest and appropriate treatment.
- Individual factors: Several individual factors influence the duration of pain. Some individuals may experience shorter pain durations due to improved healing or a positive response to treatment, while others may have prolonged pain durations due to complications such as other spinal problems.
- Type of treatment: The duration of pain also depends on the type of treatment and the individual’s response to it. Some individuals may experience rapid improvement with appropriate treatments like physical therapy, anti-inflammatory medications, and rehabilitation exercises, while other cases may continue to experience pain if there is no favorable response to treatment or if surgery is required.
- Adherence to medical advice: It is crucial for the patient to adhere to the advice provided by their physician and physical therapist. These recommendations may include appropriate rest, avoiding activities that exacerbate pain, and regular practice of rehabilitation exercises.
The duration of pain in herniated disc cases depends on various factors, and a specific timeframe for its duration cannot be determined. It is essential to understand that pain may be temporary and can improve with proper treatment and medical care. If pain persists for an extended period or worsens, it is advisable for the individual to consult a physician for an assessment and appropriate treatment, including potential additional procedures such as surgery.
When is herniated disc considered serious?
A herniated disc is a condition that affects the spine and the spinal discs that act as shock absorbers between the vertebrae. It can be mild in some cases and not pose a significant threat, but in other cases, it can be serious and require immediate attention. In this article, we will discuss when a herniated disc is considered serious and the signs to watch out for.
When is a herniated disc considered serious?
Compression of the spinal nerves or nerve roots: When a herniated disc slips between the vertebrae and exerts significant pressure on the spinal nerves or the nerve roots branching from the spinal cord, it can be considered serious. This pressure can cause severe pain, numbness, tingling, and even loss of sensory or motor function. If there are symptoms such as loss of bowel or bladder control, this is considered an emergency and requires immediate medical consultation.
Chronic and recurrent pain: If you have back or neck pain resulting from a herniated disc, and this pain is chronic and does not improve with conventional treatments or regularly returns, it may indicate the seriousness of the condition. Consultation with a specialized physician is necessary for further evaluation and care.
Persistent numbness or muscle weakness: If there is persistent numbness or muscle weakness in the affected part of the body, this indicates significant nerve compression and severe tissue damage. This can be serious and may require immediate medical assessment.
Loss of bowel and bladder control: If you notice loss of control over bowel or bladder functions, this can be a sign of significant pressure on the spinal nerves in the herniated area. Immediate medical care is necessary.
Treatment and prevention:
If a herniated disc is considered serious, it may require surgical intervention to repair the herniated discs or relieve nerve pressure. However, in less severe cases, herniated discs can be treated through physical therapy, medications, and rehabilitation exercises. To prevent the condition from worsening or occurring, individuals should take precautions to avoid injuries, maintain a healthy weight, and engage in regular physical exercise.
Tips for those suffering from a herniated disc:
If you are suffering from a herniated disc, the challenges you face can be distressing and painful. A herniated disc can cause back or neck pain, numbness, weakness, and impact your daily quality of life. However, there are some tips that can help you manage this condition and reduce pain. In this article, I will provide you with some tips for individuals dealing with a herniated disc.
- Consult Your Doctor:
The first important step is to consult your doctor or a healthcare professional specialized in treating spinal problems. The doctor will provide the necessary assessment to understand your condition and its severity, and will offer you appropriate treatment options. Treatment may include physical therapy, medications, epidural injections, and, in some cases, surgery.
- Rest:
Rest is essential for pain relief and recovery. A firm mattress and supportive pillows can help alleviate pressure on the affected spine. Try to avoid strenuous activities and lifting heavy objects until you heal.
- Physical Therapy:
Physical therapy can be effective in strengthening the muscles surrounding the spine and increasing flexibility. A physical therapist can guide you through specific exercises and posture-improving techniques to enhance your condition and reduce pain.
- Medications:
Doctors may prescribe anti-inflammatory drugs and pain relievers to alleviate pain and inflammation. Consult your doctor before taking any medication for necessary advice.
- Rehabilitation Exercises:
Rehabilitation exercises target strengthening the muscles around the spine and improving its stability. These exercises can help reduce the risk of recurrent herniation and enhance back strength.
- Healthy Weight:
If you are overweight, it can negatively impact your spine. Managing your weight and maintaining a healthy weight can reduce the gravitational pressure on your spine and alleviate pain.
- Prevention Guidelines:
After recovery, make sure to follow prevention guidelines to avoid recurrent herniation. This includes avoiding improper heavy lifting and maintaining good postures while sitting and standing.
- Rest and Warm-Up:
Before engaging in any physical activity, make sure to do warm-up and stretching exercises to avoid tissue tears and reduce the risk of injury.
- Emotional Consultation:
Dealing with pain and psychological distress may require seeking emotional support or psychological counseling to help you cope with the condition.
- Collaborate with a Specialized Medical Team:
You may need to work with a specialized medical team that includes an orthopedic doctor, physical therapist, and a psychologist if the pain is chronic and severe.
Balancing activity, rest, and healthcare is essential in managing herniated disc. Remember that each case is unique and requires individualized care. Consult your doctor for an appropriate treatment plan and follow the provided advice to alleviate pain and enhance your quality of life.
What Are the Causes of Lumbar Disc Herniation?
Lumbar disc herniation, also known as disc herniation, is a condition that affects the spine and the intervertebral discs that act as shock absorbers between the vertebrae. Lumbar disc herniation can occur due to several different causes. In this article, we will explore the most important reasons that may lead to lumbar disc herniation.
- Aging: Aging is one of the most common factors in the occurrence of lumbar disc herniation. Over time, the intervertebral discs in the spine begin to lose their flexibility and deteriorate. This deterioration makes the discs less able to bear and absorb load, increasing the risk of herniation.
- Stress and Severe Pressure: Repeated stress or severe pressure on the spine can increase the risk of lumbar disc herniation. This pressure can result from strenuous physical activities, such as improper heavy lifting, or from continuous pressure on the spine during long periods of sitting.
- Acute Injuries: Acute injuries to the spine, whether from car accidents, falls, or intense sports, can lead to lumbar disc herniation. These injuries can displace the intervertebral disc from its natural position.
- Genetic Factors: There may be genetic factors that make some individuals more susceptible to lumbar disc herniation than others. If there is a family history of disc herniation, you may have a higher risk of developing this condition.
- Smoking: Some research suggests that smoking can increase the risk of lumbar disc herniation. Smoking affects the blood flow to the intervertebral discs and reduces their ability to heal.
- Diseases and Disorders: Some medical conditions, such as arthritis, multiple sclerosis, and connective tissue diseases, can increase the likelihood of lumbar disc herniation.
- Excess Weight: Excess weight can exert additional pressure on the spine and increase the risk of disc herniation. Excess weight can lead to faster deterioration of the intervertebral discs.
- Neurological Disorders: Some disorders of the nervous system, such as diabetes, can affect the ability of intervertebral discs to retain moisture and flexibility, increasing the risk of herniation.
Understanding the causes of lumbar disc herniation is important for taking preventive measures and receiving appropriate treatment. If you are experiencing symptoms of lumbar disc herniation or suspect you have this condition, it is essential to consult a specialist for assessment and proper treatment.
What Is the Treatment for Lumbar Disc Herniation?
The treatment for lumbar disc herniation requires an initial assessment of the patient’s condition and the severity of symptoms. There are several possible treatment options for this condition, including traditional treatments, physical therapy, and surgical procedures. In this article, we will detail these options and when each one may be used.
- Rest and Self-Care: For mild and non-severe cases of lumbar disc herniation, self-care can be effective. This includes:
- Bed Rest: The patient should avoid strenuous activities, fatigue, and should lie on a flat and firm bed.
- Applying Ice: A bag of ice wrapped in a soft cloth can be placed on the affected area for 15-20 minutes several times a day to reduce inflammation and alleviate pain.
- Medications: The doctor may prescribe certain medications to help alleviate pain and inflammation. These medications may include:
- Pain relievers such as aspirin and ibuprofen.
- Non-steroidal anti-inflammatory drugs (NSAIDs).
- Pain medications like opioids in cases of severe pain.
- Physical Therapy: Physical therapy is an important option in the treatment of lumbar disc herniation. A physical therapist provides exercises and techniques to improve the strength of the muscles surrounding the spine and increase flexibility. It can also help improve body posture and alleviate pain.
- Epidural Injections: If pain does not respond to medications and physical therapy, the doctor may perform epidural injections in the affected area. These injections usually contain a combination of pain-relieving, anti-inflammatory, and steroid medications to reduce inflammation and pain.
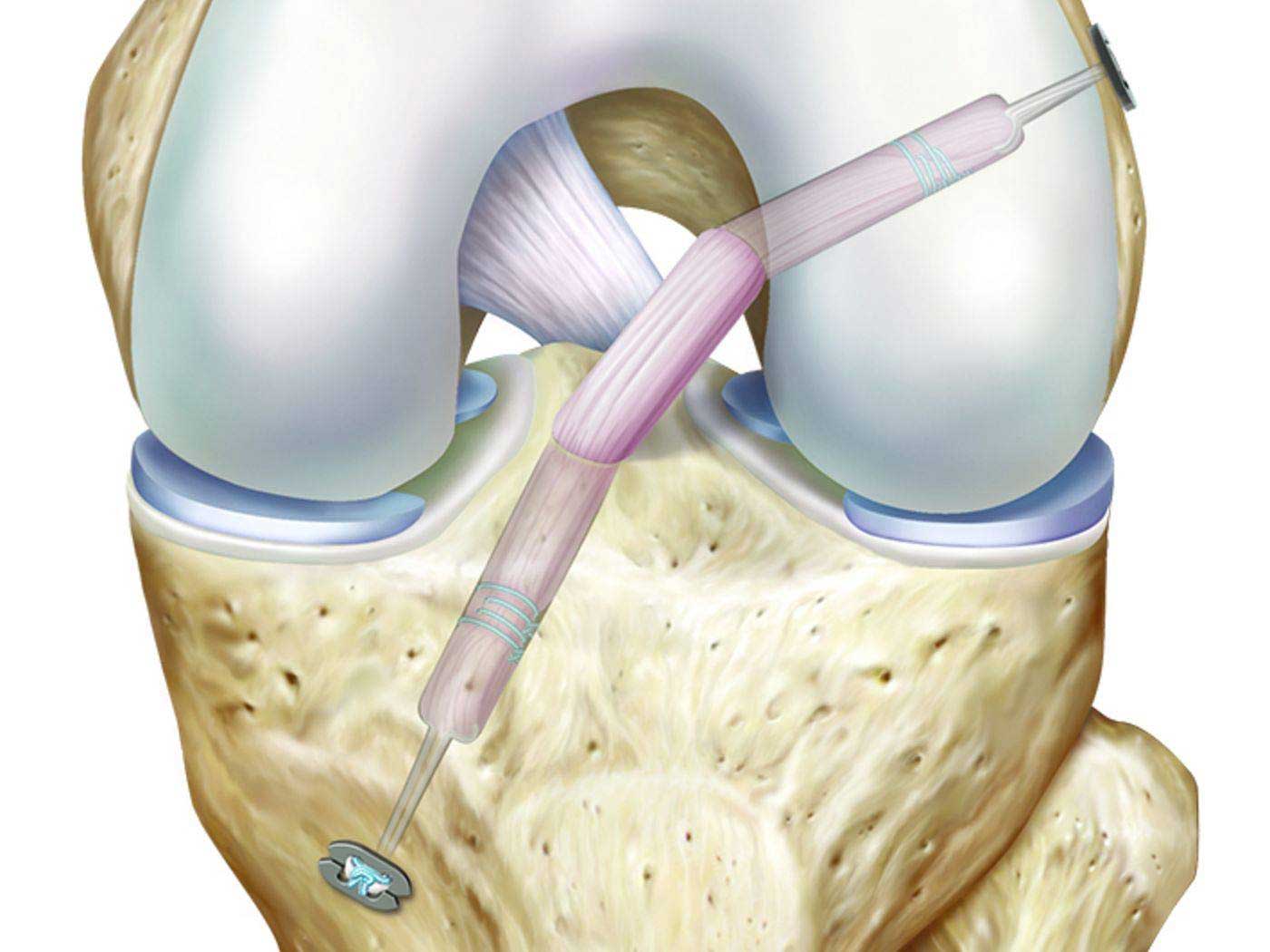
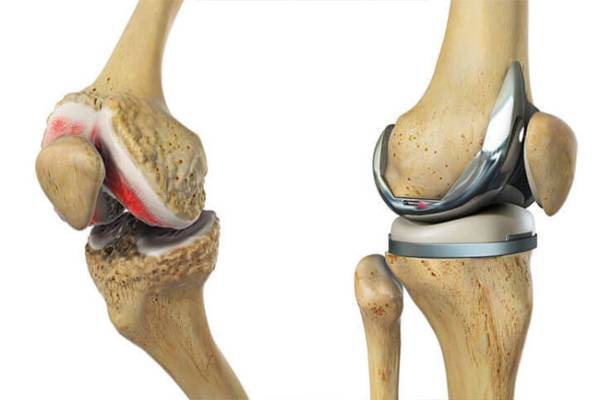
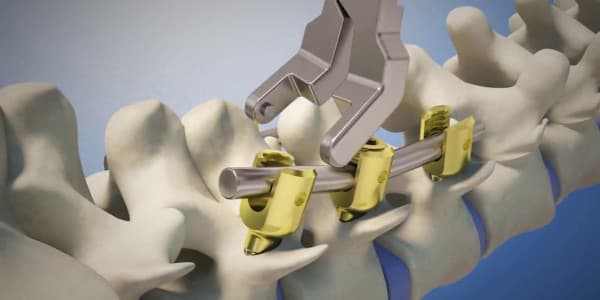
- Surgery: If previous treatments are ineffective or if there are serious issues such as nerve compression, loss of nerve function, or significant deterioration in the condition, surgery may be necessary. Discectomy is one of the common procedures for treating lumbar disc herniation. This surgery involves removing the damaged intervertebral disc or a portion of it to relieve pressure on the nerves and surrounding tissues.
- Rehabilitation Exercises: After surgery or during the physical therapy phase, rehabilitation exercises can be highly beneficial for regaining strength, flexibility, and overall spinal function.
- Guidance and Prevention: After treatment and recovery, the patient should follow guidance to prevent the recurrence of disc herniation. This includes avoiding activities that increase pressure on the spine and maintaining proper postures while sitting, sleeping, and regularly performing muscle-strengthening exercises.
The treatment for lumbar disc herniation depends on the severity of the condition and the patient’s needs. It is always essential to consult a specialized doctor for proper evaluation and the selection of the appropriate treatment option. Patient compliance with treatment and adherence to preventive measures play a crucial role in improving outcomes and recovery.
When is Surgical Intervention Necessary for Disc Herniation?
Surgical intervention for disc herniation is a procedure used when there is severe deterioration in the patient’s condition or when there are serious issues that require surgical treatment. Doctors must evaluate each case individually to determine when surgical intervention is necessary. In this article, we will discuss when surgical intervention is performed in cases of disc herniation.
- Loss of Nerve Function: If there is a loss of nerve function due to severe compression of the nerve roots or the spinal cord, this is a strong indication for surgical intervention. Loss of sensation or the ability to move in the lower or upper limbs indicates a serious condition that requires immediate surgery to relieve nerve compression and restore function.
- Severe and Persistent Pain: If the pain is extremely severe and persistent despite the use of traditional pain medications and treatments, surgery may be necessary. The pain may result from severe nerve compression or advanced inflammation in the herniated disc.
- Failure of Conservative Treatment: If conservative treatments such as rest, medications, and physical therapy fail to improve the patient’s condition over time, surgery may be the only available option to alleviate symptoms and prevent further deterioration.
- Permanent Numbness and Tingling: If there is permanent numbness and tingling in the limbs or any part of the body due to disc herniation and nerve compression, this indicates the need for surgical intervention to restore nerve function.
- Rapid Deterioration: In some cases, the patient’s condition may deteriorate rapidly, necessitating immediate surgical intervention. This can occur due to worsening disc herniation or nerve damage from excessive pressure.
- Paralysis: If there is any form of paralysis resulting from disc herniation and compression of the spinal cord, this requires urgent surgical intervention. Paralysis is considered an emergency condition and must be treated as soon as possible to prevent permanent damage.
In the end, the patient’s need for surgical intervention should be determined based on a comprehensive evaluation by the treating medical team. If you are experiencing symptoms of disc herniation and are considering surgery, you should consult with your treating physician for advice and appropriate options for your specific case.