Is a Herniated Disc a Chronic Illness? And Can It Be Cured with Physical Therapy?
Is a Herniated Disc a Chronic Disease?
Is a herniated disc a chronic disease or can it be cured?
- Definition of a Herniated Disc: A herniated disc is a condition where part of the intervertebral disc, which is made of cartilage, slips out of place and presses on the spinal nerves, causing pain and numbness in the back and extremities.
- Answering the Question: Is a herniated disc a chronic disease? In a few cases, a herniated disc can be considered a chronic condition that may lead to paralysis if not treated properly. However, symptoms can often be improved and alleviated through conservative treatment and adherence to preventive advice.
- Factors That Increase the Likelihood of a Herniated Disc:
Rheumatic diseases. Repetitive strenuous work. Advancing age. Working in improper positions for extended periods. Excessive obesity.
- Tips for Preventing a Herniated Disc:
Maintain good body posture while sitting and standing. Strengthen the back and abdominal muscles to support the spine. Avoid sitting for long periods without movement. Follow a healthy and balanced diet to lose excess weight.
- Available Treatments for a Herniated Disc:
Conservative treatment: Includes rest, avoidance of aggravating activities, and the use of ice or heat to relieve pain. Physical therapy: Involves exercises to strengthen muscles and increase flexibility to improve spinal stability. Medication: May be prescribed to alleviate pain and reduce inflammation in the affected area. Surgical treatment: Recommended in advanced and severe cases that respond poorly to conservative and physical therapies.
- Exercising with a Herniated Disc: For individuals with a herniated disc, it is advised to engage in low-impact, aerobic exercises such as walking and swimming. Activities that increase spinal pressure, like running and weightlifting, should be avoided.
- The likelihood of a Herniated Disc Recurrence after Symptoms Disappear: Even if symptoms disappear, patients should be aware that a herniated disc may not be completely healed and that the disc may not return to its normal position. However, the condition may improve, and symptoms may lessen thanks to certain mechanisms in the body involving the effect of anti-inflammatory substances and the stimulation of immunity to deal with the condition.
In conclusion, patients with a herniated disc should consult a specialist for proper diagnosis and treatment. A herniated disc can be a chronic condition in some cases, so conservative treatment and preventative advice should be followed to improve symptoms and reduce potential risks.
What is the recovery time for a herniated disc?
A herniated disc is a common condition that affects the vertebrae and causes painful symptoms. The recovery time from a herniated disc varies among individuals and depends on several factors, including the severity of the condition and the type of treatment followed. In this article, we will provide an overview of the typical recovery time for herniated disc cases.
- Typical Recovery Duration: Generally, herniated disc cases take about 4-6 weeks to heal. Nonetheless, patients should gradually return to normal activity after the recovery period has ended. It should be noted that full recovery milestones should be achieved before resuming routine activities.
- Symptoms that Fade Over Time: After the healing period, the symptoms associated with a herniated disc should begin to gradually diminish. Notable symptoms that disappear with healing include muscle spasms and pain in the back and neck.
- Specific Treatments Required: The normal recovery duration can be affected by the specific treatment the patient undergoes. Treatment may include pain relievers and sometimes cortisone injections. Patients must adhere to the specified treatment and follow the instructions of the specialist to speed up healing and reduce complications.
- Precautions and Lifestyle Adjustments: It is important for patients to follow the necessary advice and precautions to accelerate the healing time from a herniated disc. These precautions may include performing rehabilitative exercises, ensuring good body posture while sitting and sleeping, and avoiding harmful activities that put pressure on the spine.
Can complete recovery from a herniated disc be achieved? Yes, complete recovery from a herniated disc is possible. However, it should be known that the healing process may take an extended time and varies based on individual conditions and the severity of symptoms. Therefore, it is recommended to stay in contact with the treating physician and monitor the progress of improvement during the recovery period.
Online data suggests that the recovery period from a herniated disc ranges between 4-6 weeks. Nonetheless, many factors must be taken into account, including the severity of the condition and the type of treatment required. Patients should adhere to the doctor’s instructions and follow a healthy lifestyle to expedite the healing process.
Is recovery from a herniated disc possible with physical therapy?
Herniated disc is a painful and chronic condition that affects many people, but can it be cured with physical therapy? We will answer this question and provide you with some important information on this topic.
Physical therapy as an effective method: Physical therapy is considered one of the most common and preferred methods for patients to treat a herniated disc. It aims to control pain, improve body movement, and muscle strength.
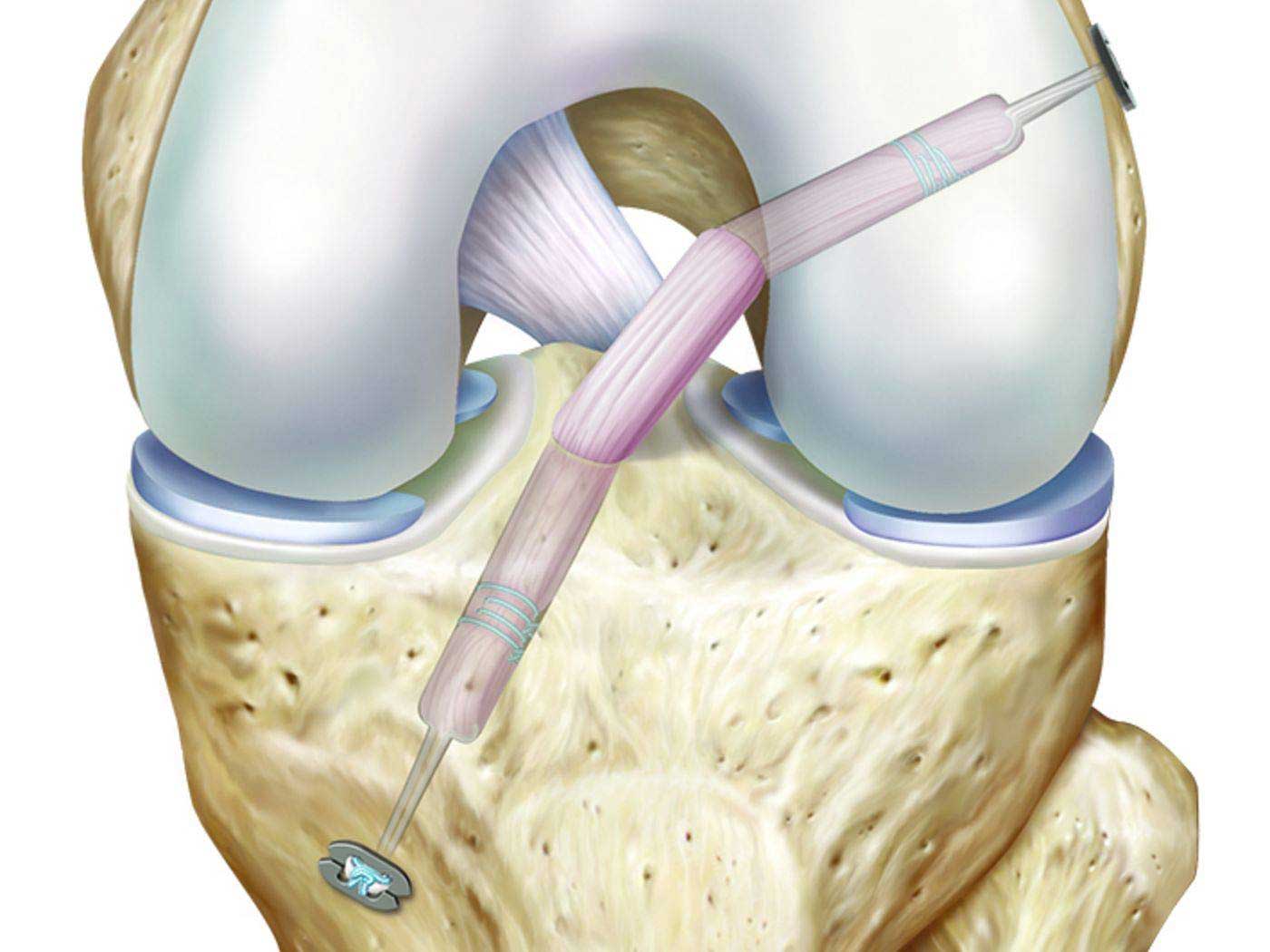
Techniques used in physical therapy: Medical examination and the assessment of movement and strength are used to determine the appropriate physical therapy techniques. Among these techniques are:
- Massage: Massage helps relieve pain and reduce tension in the muscles surrounding the affected disc.
- Therapeutic exercises: These exercises aim to strengthen the muscles around the affected disc and improve flexibility and movement.
- Heat and cold therapy: Heating and cooling are used to reduce inflammation and relieve pain.
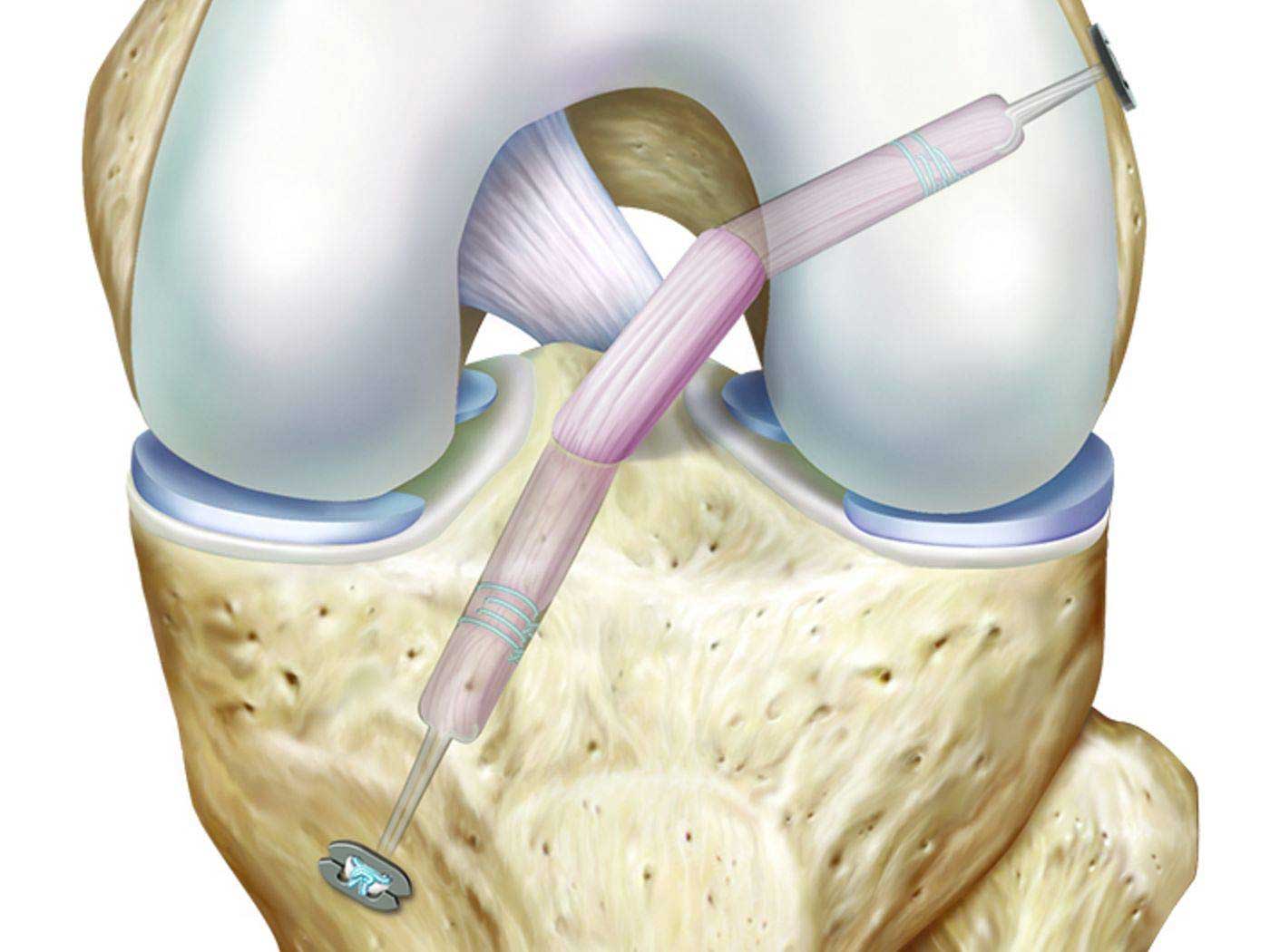
- Therapeutic surgery: This surgery is used to relieve pain and improve musculoskeletal system functions.
Benefits of physical therapy in treating a herniated disc:
- Physical therapy has several potential benefits in treating a herniated disc: Improving movement and flexibility in the spine. Strengthening the muscles surrounding the affected disc. Reducing pain and inflammation in the affected area. Helping in the patient’s return to normal daily life.
- Doctors’ orientations in physical therapy for herniated disc: Medical laser: Used to alleviate pain and reduce swelling in the affected area.
- Ultrasound: Used to achieve a strong therapeutic effect in the damaged tissues. Aquatic therapy: Performed in warm water, which helps reduce pressure on the spine and alleviate pain.
- Patience and Commitment: Physical therapy must be a continuous and ongoing process, as improvement in condition requires time and effort. For some, healing may take weeks or even months to fully recover.
Although physical therapy can be effective in improving herniated disc conditions, patients should consult with their treating physician to evaluate their specific cases and determine the best treatment for them. It should also be taken into account that other procedures may be necessary in severe cases of herniated discs.
Before applying any physical or surgical therapy, it is recommended to consult a specialist for an accurate diagnosis and to determine the appropriate treatment for your case.
Is a herniated disc considered a disability?
Cases in which a person suffers from a spinal disc herniation are common injuries that can cause many complications. Although a herniated disc is not necessarily a definitive barrier for the affected person, it can cause symptoms that may affect their daily life.
Patients with a herniated disc experience severe pain in the slipped vertebrae and may also feel numbness in certain areas of the body. Questions may arise as to whether this herniation is considered a disability and whether it will lead to paralysis.
In fact, a herniated disc is a medical condition and not an official classification of disability. However, the impact of a herniated disc depends on the severity of symptoms and complications experienced by the individual. In some severe cases, a herniated disc can lead to pressure on the nerves, which impedes the movement of nerve signals, causing numbness in the limbs and potentially affecting the ability to walk normally.
Nevertheless, it should be noted that many cases of herniated discs can be managed with appropriate treatment and rehabilitation. The treatment of a herniated disc may include medical therapies such as medication and physical therapy sessions, and in some advanced cases, surgery may be required.
In any case, a person suffering from a herniated disc should consult with a spine specialist or a qualified physician to individually assess their condition. This may involve medical tests and imaging to determine the degree of the herniation and its impact on the individual.
In conclusion, although a herniated disc is not necessarily a disability, it can affect the life of the person suffering from it. It is crucial that the patient follows the appropriate medical advice and receives the proper treatment to improve their condition and alleviate symptoms.
Are there cases cured of disc herniation?
5 astonishing cases cured of disc herniation:
- A case healed through physical therapy: Mrs. Fatima suffered from severe back pain due to a lumbar disc herniation. She decided to try physical therapy and work on strengthening her back muscles and improving flexibility. After several weeks of physical therapy and regular sessions, her pain significantly decreased and Fatima returned to her normal life without any surgical intervention.
- A case healed with non-surgical intervention: Mr. Ali pursued non-surgical treatment for his cervical disc herniation. This treatment included physical therapy sessions, rehabilitative exercises, and avoiding activities that increase pressure on the neck. Thanks to this treatment, Ali’s condition gradually improved and he managed to eliminate the pain and fully recover his movement.
- A case healed with medication: Mr. Mohammed suffered from intense back pain due to a disc herniation. Medication was prescribed to alleviate the pain and inflammation. After a short period of treatment, Mohammed noticed a remarkable improvement in pain and regained a significant part of his daily functions.
- A case healed with surgical intervention: Mrs. Nadia’s situation was complex as she suffered from a cervical disc herniation causing pain and weakened control over her arms. After traditional treatments failed, Nadia decided to undergo surgery to remove the damaged disc. Post-surgery, Nadia returned to normal life and regained her ability to perform daily activities without pain.
- A case healed thanks to integrated treatment: Mr. Ahmed suffered from lumbar disc herniation in his back, experiencing acute pain and numbness in his legs. Ahmed resorted to an integrated treatment that includes medication, physical therapy, healthy nutrition, and regular physical activity. Gradually, Ahmed’s condition improved and he was able to return to his normal life without continuous pain.
Certainly, disc herniation cases can vary according to their severity and nature. It is important to consult doctors and explore the appropriate treatments for each individual case.
These amazing cases give hope to people suffering from disc herniation pain and remind us that full recovery may be possible in some instances. We must remember that each case is individual and may need different treatment according to its own circumstances. Therefore, it is essential to consult specialized doctors to get the correct diagnosis and necessary guidance for the appropriate treatment.
When is surgery necessary for a herniated disc?
Individuals may experience back pain due to herniated disc disorders, which involve issues with the discs between the vertebrae. Usually, this pain can be alleviated through painkillers and exercises designed to strengthen and stretch the spine. However, if the space between the vertebrae narrows due to the disc pressing on nerves, surgical intervention may be necessary.
In this article, we will review some important points to determine when surgery is necessary for herniated disc cases:
- Persistent pain: If the patient suffers from ongoing pain despite taking painkillers and performing spinal stretching exercises, the doctor should consider surgery.
- Discogenic pain: If the pain worsens when standing or using the foot, this may indicate a herniated disc that requires immediate surgical intervention.
- Motor deficiency: If the patient is having difficulty moving and is unable to walk, this may be evidence of the need for surgical intervention.
- Issues with vital functions: If the herniated disc is pressing on nerves responsible for bladder and bowel functions, the surgeon must intervene to prevent chronic problems.
- Recurrence of the condition: In some cases, a herniated disc may occur a second time after non-surgical treatment. In this case, surgical intervention may be the best solution to prevent recurrence.
- Medical examination assessment: The doctor must comprehensively evaluate the patient’s medical exams before deciding to perform surgery. These examinations may include X-rays, MRI scans, and other tests to determine the state of the herniated disc.
Given that this information is derived solely from online data, patients should consult specialists to assess their individual cases and make the appropriate decision. Surgical intervention may be the best treatment in some cases, but this depends on the specialist’s evaluation and the circumstances of each case
How to cope with a herniated disc?
- Follow a back and surrounding muscle strength exercise program: Most people can alleviate herniated disc pain by following an exercise program designed to strengthen the back and surrounding muscles. These exercises work to improve the strength of the spine and increase its stability. Practicing appropriate exercises can reduce the pressure of the disc on the nerves and improve pain.
- Use over-the-counter pain relievers: Over-the-counter pain relievers can help alleviate the pain associated with a herniated disc. Consult a doctor before taking any medication to ensure it is compatible with the overall health condition and current medication.
- Physical therapy: The doctor may recommend physical therapy to help improve movement and reduce pain. Physical therapy includes stretching, strengthening, and relaxation exercises, as well as manual therapy techniques such as massage.
- Avoid heavy operations and incorrect movements: Lifting heavy objects and strong movements that may negatively affect your spine should be avoided. It is advised to maintain a proper sitting posture and avoid positions that put pressure on the herniated disc.
- Sleep in a correct position: Sleep should be in the correct position to support the spine and reduce pressure on the herniated disc. Special pillows can be used to support the neck and back during sleep.
- Engage in suitable sports: Engaging in light exercises and gentle sports such as walking can help relieve pain and enhance muscle strength. Consult a doctor before starting any sports activity to ensure it is suitable for your health condition.
It is important to consult a doctor to accurately assess the condition of the herniated disc and determine the appropriate treatment options. Always remember that adherence to treatment and necessary self-care can help improve the condition and relieve symptoms.
Does rest help in treating a herniated disc?
Yes, rest can help in the treatment of a herniated disc if implemented correctly. In cases of a herniated disc, bed rest and avoiding strenuous activities and excessive movements are an important part of the treatment. Rest helps to reduce the pressure on the herniated disc and can assist in alleviating pain and inflammation. However, it is essential to consult a doctor or a physical therapist before implementing any type of treatment to ensure that it is suitable for the individual’s condition and that there are no other complications.
How should a patient with a herniated disc sleep?
A herniated disc is a medical condition that causes pain and discomfort for those affected. Patients deal with difficulties in sleeping due to the pain and accompanying symptoms. However, there are certain correct sleeping positions that can help alleviate pain and improve the quality of sleep for patients with a herniated disc.
Here is a list of the correct sleeping positions for patients with a herniated disc:
- Lying on the back with a pillow:
- Lie on your back and slightly bend your knees.
- Place a medium-sized pillow under your knees for support.
- Put a thin pillow under the abdomen and hips area to raise the middle part of your body.
- Preferably use a flat pillow for your head while sleeping on your back, but you can sleep without a pillow if that is more comfortable for you.
- Sleeping on one side in the fetal position:
- If sleeping on your back is uncomfortable, try sleeping on one side of your body in the fetal position.
- Bend your knees slightly and bring them up in front of you.
- Place a comfortable pillow under your head and another between your knees for support.
- Sleeping on the stomach with proper positioning:
- Generally, sleeping on the stomach is not recommended for patients with a herniated disc, but it can be suitable for some people.
- Place a thin pillow under the abdomen and hips to support the middle part of your body.
- You can use a flat pillow for your head or sleep without a pillow.
Whatever sleeping position you choose, you should feel comfortable and supported. Consult your doctor before trying any changes to your sleeping position. They may have more specific advice for your condition.
Important reminder: It should be noted that this information is derived from online sources and is not a substitute for professional medical consultation. Before implementing any changes in this regard, it is advised to consult with your treating physician to get the appropriate medical advice.
Does a herniated disc cause nerve damage?
A herniated disc is a common condition that affects many people, and it often raises the question of whether it can cause nerve damage. In this article, we will address this issue and provide you with the basic information about herniated discs and their impact on the nerves.
Effects of a herniated disc:
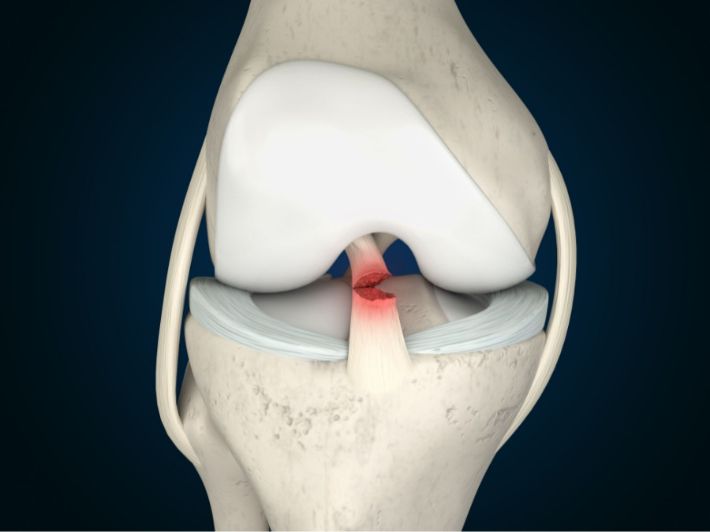
- A herniated disc can cause compression of the surrounding nerves, which can result in nerve damage and disruption of their normal function.
- In cases of a large herniation that compresses the nerves in the back area, it may affect both sides of the body and cause dysfunction in the digestive system, loss of bladder and bowel control, and even sexual dysfunction.
Causes of a herniated disc:
- A herniated disc occurs as a result of pressure on the spinal cord nerves due to the slipping of the intervertebral disc.
- It can occur due to activities that require continuous sitting for long periods, such as office work, as well as squatting and lifting heavy loads.
- It may also occur as a result of sudden movements or stress on the lower spine, such as when lifting heavy objects or falling.
- Research indicates that the presence of genetic mutations may increase the risk of a herniated disc in some people.
Symptoms of a herniated disc:
- Symptoms of a herniated disc vary depending on the location of the herniation and the types of tissues affected.
- Symptoms may include varying pain in the neck or back, with an increase in pain when moving or sitting for long periods.
- Pain may be accompanied by numbness in the affected limbs and weakness in muscular strength.
- In some severe cases, permanent paralysis or nerve damage may occur due to the herniation pressing on important nerves for bodily functions.
- The likelihood of herniated discs increases with age, as the discs wear down over time.
- Excess weight is a contributing factor in increasing pressure on the discs in the back.
The following table illustrates some of the factors influencing the risk of a herniated disc:
Factors Influencing the Risk of a Herniated Disc: [Note: The original text did not include the table content, so it is not provided here.]
In general, a herniated disc can cause nerve damage and negative effects on bodily functions as explained above. It is essential to consult a specialist doctor in case of symptoms related to a herniated disc for early diagnosis and to establish an appropriate treatment plan.
Can Cartilage Rebuild Itself?
Cartilage is an essential part of the human body, particularly in the joints, serving as an interface for absorption and protection between bones. In the past, it was believed that cartilage could not naturally rebuild itself, but with the advancement of research and studies, it has been discovered that there is some regenerative capacity in cartilage.
In this list, we will review some facts and prevalent information about the possibility of cartilage rebuilding:
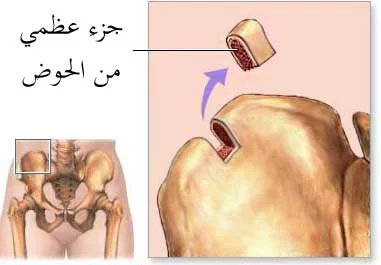
- Cartilage Regeneration in Joints: Recent research shows that humans can regenerate cartilage in the joints, not only salamanders as previously thought. For instance, researchers at Duke University in the United States discovered that joint cartilage could regenerate itself through a mechanism similar to that found in creatures like salamanders and zebrafish.
- Factors Enhancing Regeneration: There are certain factors that may help enhance the cartilage’s ability to regenerate. According to research, this process can be enhanced by promoting regulatory molecules that contribute to the rebuilding of deteriorated cartilage. Once these molecules are identified, they can be reintroduced to individuals suffering from cartilage issues, thereby stimulating the natural regeneration process.
- Continuing Treatment and Prevention: It is not sufficient to rely solely on the natural process of cartilage regeneration; appropriate treatment must be followed, and preventive measures must be taken to ensure the comfort of the cartilage and to prevent the exacerbation of pain and damage. Treatment may include physical therapy and suitable exercises, in addition to avoiding excessive activities and direct injuries.
In summary, although cartilage does not fully return to its original state by itself, there is some capacity for regeneration in certain cases. This depends on the extent of injury, the type of treatment applied, and the maintenance of an appropriate health regime. It is important that the condition is monitored and care is received from specialized doctors to ensure the best healing outcomes and to maintain joint health.