What are the symptoms of herniated disc and what is the difference between it and sciatica?
Symptoms of Herniated Disc
Herniated disc, also known as a slipped disc or disc prolapse, is a common condition that affects many people. This condition is characterized by the displacement of a spinal disc between two adjacent vertebrae, which can lead to compression and irritation of the surrounding nerves, causing various painful and bothersome symptoms. Below, we will provide you with a list of the key symptoms of herniated disc:
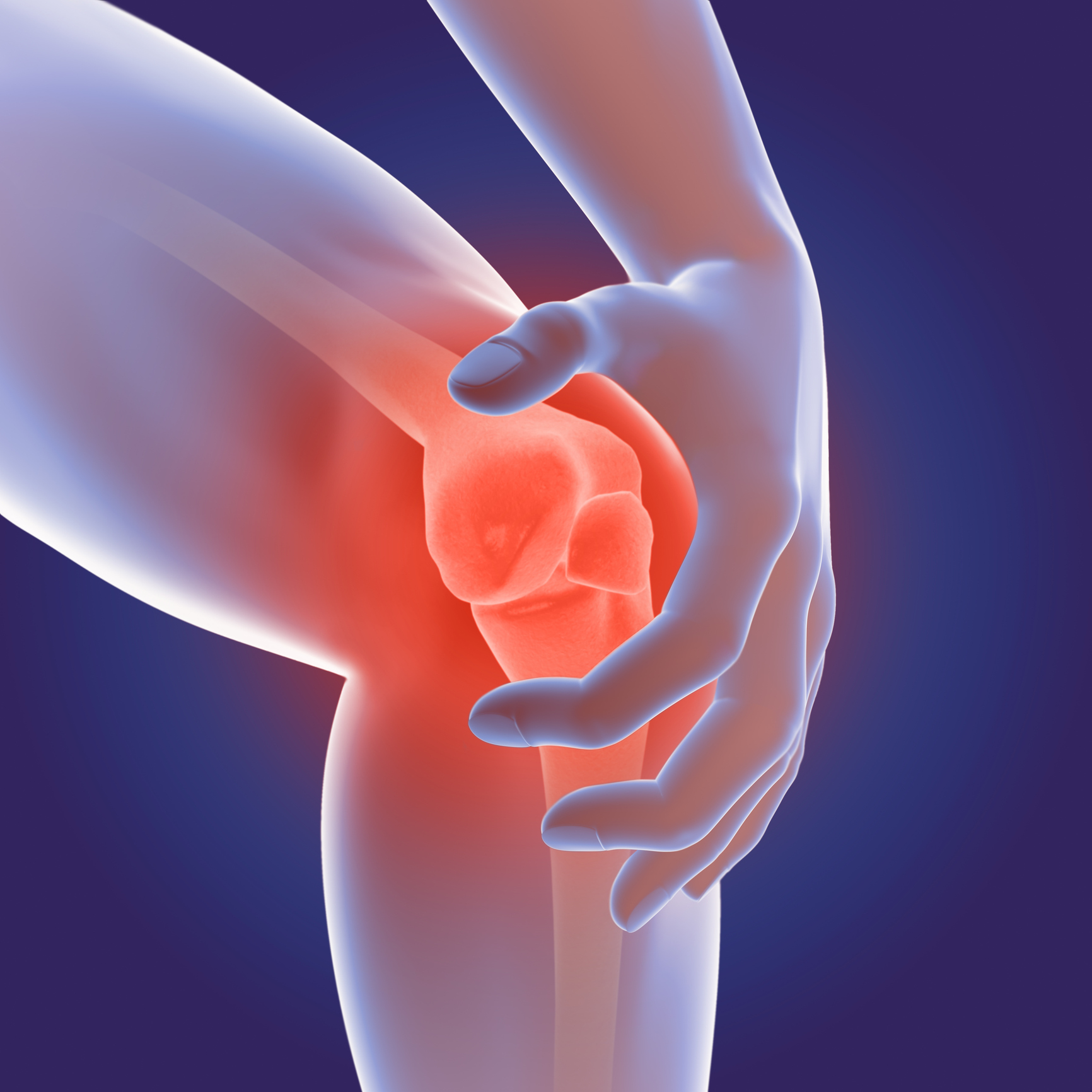
- Pain: Pain is one of the most prominent symptoms of a herniated disc. The pain can be either continuous or intermittent and may worsen with spinal movement or simple motions. It may be localized to the area of the herniated disc itself or radiate to other parts of the body, such as the arms or legs.
- Tingling and Numbness: Tingling and numbness are common symptoms of herniated disc. When the herniated disc presses on the nerves, you may experience tingling or numbness in the extremities surrounding the affected spinal column, such as the hands or feet.
- General Muscle Weakness: Herniated disc can lead to general muscle weakness in the affected area. You may have difficulty performing everyday movements, such as sitting or standing, and this overall weakness can impact your ability to engage in sports or lift heavy objects.
- Difficulty Standing or Sitting: Some individuals with a herniated disc experience difficulty when trying to stand or sit. Attempting to stand or sit may increase the pressure on the affected nerves, leading to increased pain and tension.
- Acute and Sudden Pain: Herniated disc may be accompanied by acute and sudden back pain. This pain can be characterized by its severity and rapid exacerbation.
Knowing the symptoms of herniated disc is important for recognizing your condition and initiating appropriate treatment. If you are experiencing any of these symptoms, it is important to consult your physician for a precise diagnosis and suitable treatment.
Can Herniated Disc Be Cured Completely?
Many individuals suffering from herniated discs, whether in the neck or back, wonder if a complete recovery from this condition is possible. In this article, we will explore this common question and highlight non-surgical interventions that can help achieve recovery.
Non-Surgical Interventions:
In collaboration with Dr. Amr Amal, several non-surgical interventions are offered to help alleviate the pain associated with a herniated disc. These interventions include:
- Physical Therapy: This involves targeted exercises and physical therapy sessions to strengthen the muscles surrounding the herniated disc and improve spinal alignment.
- Epidural Injections: When chronic pain persists and does not improve with other interventions, epidural injections can be used to relieve pain and reduce swelling.
- Medication: Anti-inflammatory and pain medications are used to alleviate symptoms associated with a herniated disc.
The Possibility of Complete Recovery:
It is important to note that the possibility of complete recovery from herniated disc pain depends on several factors, including:
- Severity of the Condition: The recovery period depends on the extent of the disc and nerve involvement. Individuals with severe or advanced cases may require a longer recovery time.
- Body’s Response: The body’s response to different treatments can vary, and there may be differences in improvement among individuals.
- Lifestyle Improvement: Healthy habits and lifestyle choices can play a significant role in achieving complete recovery. Maintaining good sitting posture, getting adequate sleep, and engaging in appropriate exercises are important for the recovery process.
Yes, it is possible to achieve complete recovery from cervical and lumbar herniated disc pain through appropriate non-surgical interventions. However, patients should be prepared to wait for a suitable period of time for full improvement. Medical evaluation with a specialist is necessary to determine the most appropriate treatment approach based on the patient’s condition.
Can Herniated Disc Progress?
Herniated disc is a common health issue that affects many people. It is important to know whether this condition can progress and lead to more serious problems. In this article, we will provide an overview of the likelihood of herniated disc progression.
Early Diagnosis: Early diagnosis of a herniated disc plays a crucial role in preventing its progression into more serious issues. If the condition is detected in its early stages, measures can be taken to promote healing and prevent the worsening of symptoms.
Contributing Factors: There are certain factors that can increase the likelihood of herniated disc progression. For example, weak core muscles, poor posture, psychological stress, and increased spinal pressure can contribute to the worsening of the condition.
Early Treatment:
When a herniated disc is diagnosed, treatment is directed towards improving symptoms and promoting healing. However, if treatment is delayed or not properly implemented, it can lead to the progression of the condition and worsening of the problem.
Symptom Worsening:
Worsening of symptoms may indicate the progression of a herniated disc. For example, if the pain intensity increases or new symptoms such as limb numbness or muscle weakness appear, it could be a sign of the condition deteriorating.
Advanced Diagnostic Tests:
In some cases, new developments may necessitate additional diagnostic tests such as MRI or CT scans. These tests provide a more detailed image of the herniated disc condition and assist in determining the appropriate treatment plan.
Prevention and Long-Term Treatment:
Most individuals with a herniated disc respond well to conservative treatment and physical therapy. However, sufficient time should be taken for recovery, and core muscle strengthening exercises should be practiced, along with maintaining proper body posture. This helps prevent problem progression and future painful episodes.
In summary, the progression of a herniated disc depends on several factors, including early diagnosis, appropriate treatment, and health maintenance. It is important for individuals dealing with this condition to consult their healthcare providers and follow the appropriate medical guidance to avoid problem progression and improve their quality of life.
How Long Does Herniated Disc Pain Last?
Herniated disc is a condition caused by damage to the discs surrounding the spinal vertebrae. The most common symptoms of herniated disc are pain, numbness, and weakness in the lower limbs. Many people wonder about the duration of pain associated with herniated disc. In this article, we will shed light on how long the pain may last for individuals with herniated disc.
Factors Affecting the Duration of Pain:
- Severity of Herniated Disc: The pain may persist for a longer period if the herniated disc is severe. If there is significant pressure on the nerves, the patient may require an extended recovery period.
- Type of Treatment: The success of treatment depends on the use of appropriate therapies. Treatment options may include pain-relieving medications, physical therapy, rehabilitation exercises, injections into the affected area, and, in some cases, surgery.
- Individual Response: The body’s response to treatment varies from person to person. Some patients may experience rapid improvement after starting treatment, while others may require a longer recovery time.
Average Duration of Pain:
There is no definitive answer to the duration of pain in cases of herniated disc, as it varies from person to person. However, we can provide a reasonable estimate based on the experiences of previous patients.
In general, the pain associated with herniated disc can last anywhere from several weeks to several months. In many cases, the pain gradually subsides with proper treatment and sufficient rest. However, some patients may require a longer period to achieve full recovery.
Important Reminder:
Consulting a specialist doctor is essential for diagnosing the herniated disc condition and determining the most appropriate treatment. Delaying treatment should be avoided, and following the doctor’s guidance accurately is crucial to achieve the best results.
Pain associated with herniated disc is common, and its duration varies based on multiple factors. It is important to collaborate with a specialist doctor and adhere to the prescribed treatment to achieve the best outcomes in recovering from this condition.
What is the Difference Between Herniated Disc and Sciatica?
Pain in the back and legs can result from various issues, and herniated disc and sciatica are among the most common causes. In this article, we will outline the differences between these two conditions to better understand them.
Herniated Disc:
A herniated disc occurs when a disc of cartilage slips between the vertebrae. Herniated disc can compress the sciatic nerve root, resulting in leg pain. Individuals with a herniated disc experience severe pain that radiates from the lower back to the leg. Herniated disc can cause pain during movement and prolonged sitting. It may lead to difficulty walking or performing daily activities normally.
Sciatica:
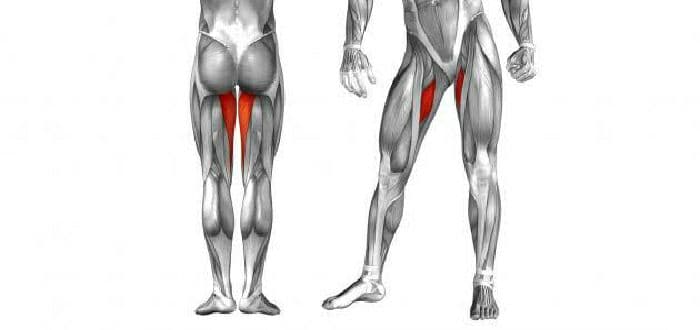
Sciatica results from inflammation, irritation, or compression of the sciatic nerve root in the lower back. People with sciatica feel pain that radiates down the leg. Sciatica may result from a herniated disc but is considered a symptom of sciatic nerve issues in general. Individuals with sciatica may experience numbness or tingling in the leg. Sciatica can be bothersome and may interfere with daily activities and movement.
Individuals experiencing back and leg pain should consult a doctor for accurate diagnosis and appropriate treatment. More complex cases may require surgical intervention, while massage and physical therapy may suffice for less severe cases. Always remember that consulting a doctor is the first step for diagnosis and necessary care.
How Is Recovery from a Herniated Disc Achieved?
Herniated disc is a painful condition affecting many individuals. Unfortunately, this condition can impact a person’s quality of life and hinder their ability to perform daily activities properly. However, can individuals with this condition fully recover and heal from it completely?
The short answer is yes, complete recovery from a herniated disc is possible. The good news is that this recovery may be achievable without the need for surgical intervention. The key to recovery lies in following certain non-surgical interventions and appropriate treatments.
Several types of non-surgical interventions are available for treating a herniated disc. Here are some of these interventions that can be implemented for recovery:
- Medication Therapy: Medication therapy involves using appropriate medications to relieve pain and inflammation. You may be directed to use non-steroidal anti-inflammatory drugs (NSAIDs) and pain relievers.
- Physical Therapy: Physical therapy includes specialized exercises that help strengthen muscles and increase spinal flexibility. Physical therapists may guide you in performing stretching and muscle-strengthening exercises, along with manual therapy and massage techniques.
- Radiation Therapy: Radiation therapy may be used to reduce pain and inflammation in the affected part of the spine. It can also be used to improve joint mobility and stimulate tissue healing.
- Stimulative Measures Therapy: Stimulative measures can be used to promote bone healing and strengthen connective tissues. These methods include treatments like laser therapy and ultrasound therapy.
It’s important to note that the duration of recovery from a herniated disc is not fixed and varies from person to person. The duration depends on the individual characteristics of each case. However, it is estimated that most cases take about 4-6 weeks to achieve full recovery.
While the mentioned treatments can be effective in many cases, some individuals may require surgical intervention in case of worsening symptoms or non-response to non-surgical treatments. It is advisable to consult a doctor to evaluate your condition and seek their advice regarding the appropriate treatment.
Overcoming a herniated disc and achieving complete recovery can be accomplished by following the appropriate non-surgical interventions and seeking proper medical guidance. Remember that rest and regular consultation with a doctor are crucial parts of treatment and achieving final recovery.
Does a Herniated Disc Show on Regular X-Rays?
Regular X-rays are a common means of detecting many medical conditions, but the question that some may ask is: can regular X-rays reveal a herniated disc?
To answer this question, let’s explore some basic information about regular X-rays and how they are used in detecting a herniated disc.
Several types of non-surgical interventions are available for treating a herniated disc. Here are some of these interventions that can be implemented for recovery:
- Medication Therapy: Medication therapy involves using appropriate medications to relieve pain and inflammation. You may be directed to use non-steroidal anti-inflammatory drugs (NSAIDs) and pain relievers.
- Physical Therapy: Physical therapy includes specialized exercises that help strengthen muscles and increase spinal flexibility. Physical therapists may guide you in performing stretching and muscle-strengthening exercises, along with manual therapy and massage techniques.
- Radiation Therapy: Radiation therapy may be used to reduce pain and inflammation in the affected part of the spine. It can also be used to improve joint mobility and stimulate tissue healing.
- Stimulative Measures Therapy: Stimulative measures can be used to promote bone healing and strengthen connective tissues. These methods include treatments like laser therapy and ultrasound therapy.
It’s important to note that the duration of recovery from a herniated disc is not fixed and varies from person to person. The duration depends on the individual characteristics of each case. However, it is estimated that most cases take about 4-6 weeks to achieve full recovery.
While the mentioned treatments can be effective in many cases, some individuals may require surgical intervention in case of worsening symptoms or non-response to non-surgical treatments. It is advisable to consult a doctor to evaluate your condition and seek their advice regarding the appropriate treatment.
Overcoming a herniated disc and achieving complete recovery can be accomplished by following the appropriate non-surgical interventions and seeking proper medical guidance. Remember that rest and regular consultation with a doctor are crucial parts of treatment and achieving final recovery.
Does a Herniated Disc Show on Regular X-Rays?
Regular X-rays are a common means of detecting many medical conditions, but the question that some may ask is: can regular X-rays reveal a herniated disc?
To answer this question, let’s explore some basic information about regular X-rays and how they are used in detecting a herniated disc.
Severe Spinal Compression: Exercises that require severe spinal compression, such as abdominal exercises involving jumping or heavy lifting, should be avoided because they can increase pressure on the affected disc and worsen symptoms.
Excessive Spinal Extension: Exercises that involve excessive spinal extension, like improper weight lifting or overstretching, should also be avoided. These movements can potentially cause further damage to the disc and lead to additional tears.
High-Impact Exercises: High-intensity strength and endurance exercises, such as heavy weightlifting or high-impact activities in various sports like fast running, can be detrimental for individuals with a herniated disc. The significant pressure and impact on the spine can exacerbate the condition.
If you have a herniated disc, it is essential to consult a physician before engaging in any physical activity. A doctor can determine the most suitable exercises for your condition and advise you on movements to avoid. Remember that maintaining gentle physical activity and movement can be beneficial for improving your condition, but exercises that increase pain and worsen symptoms should be avoided.
Which Vertebrae Are Most Prone to Herniated Discs?
Herniated discs are a common condition that affects the discs in the spine, leading to back pain, neck pain, and other body issues. Here are the vertebrae most prone to herniated discs:
Cervical Vertebrae (Neck Vertebrae): Cervical vertebrae are located in the neck region and are the second-most commonly affected vertebrae by herniated discs, following lumbar vertebrae. Cervical herniated discs occur when a disc protrudes and compresses the nerve roots between the vertebrae. This can cause neck pain and pressure on the nerves, leading to tingling and numbness in the arms and shoulders.
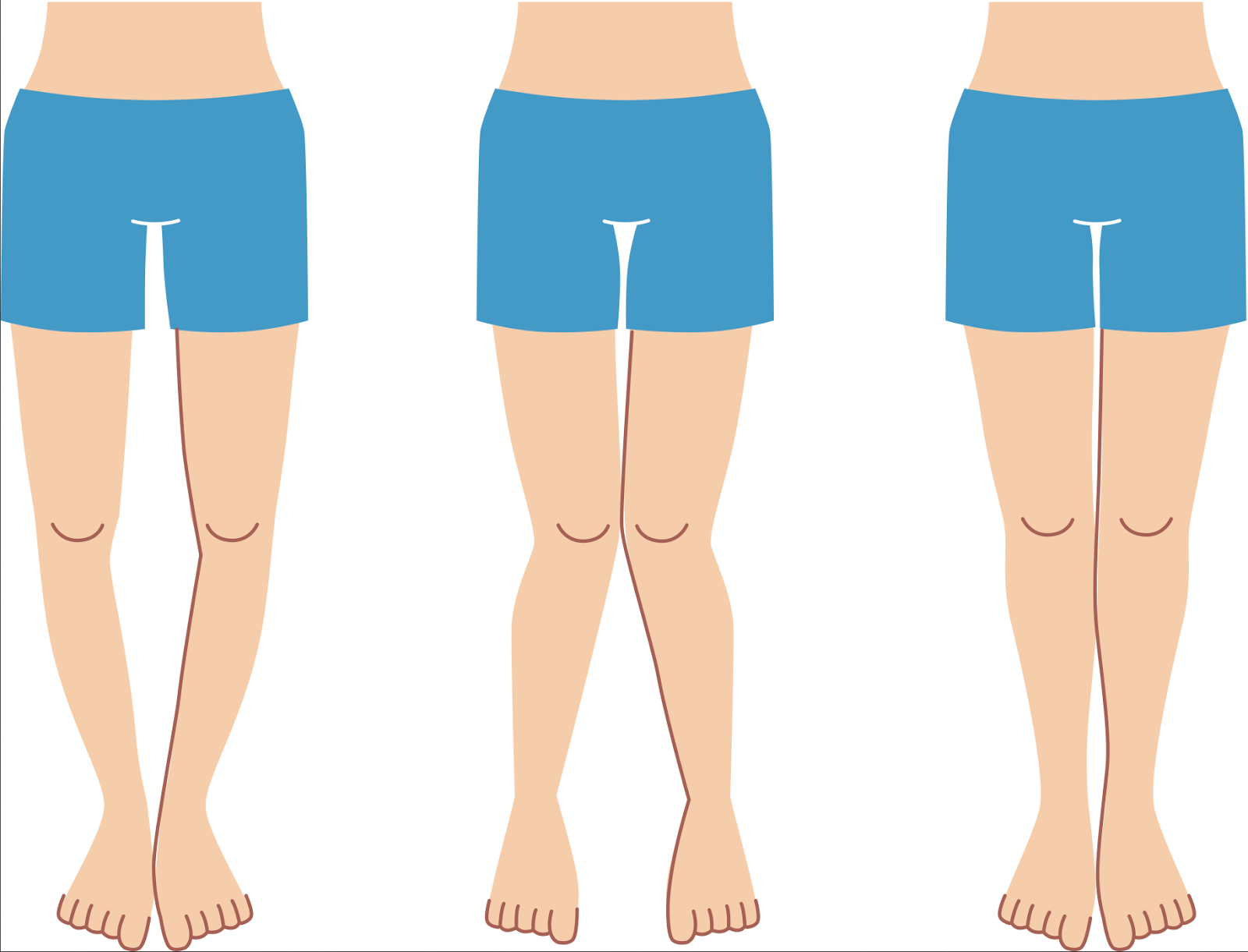
Lumbar Vertebrae (Lower Back Vertebrae): Lumbar vertebrae are located in the lower back region and are the most commonly affected vertebrae by herniated discs. Lumbar herniated discs occur when a disc becomes filled with fluid and compresses the nerve roots between the vertebrae. This can cause severe lower back pain and tingling in the legs and feet, affecting a person’s mobility and quality of life.
Sacral Vertebrae: The sacral vertebrae are a single set of vertebrae within the spinal column, located in the lower part of the spine. Although sacral vertebrae are less prone to herniated discs compared to cervical and lumbar vertebrae, a herniated disc in this area can still cause pain and numbness in the pelvis and legs, affecting a person’s ability to walk and move freely.
It’s important to note that herniated discs can occur in any vertebra in the spine, and the influencing factors and causes may vary from one case to another. If you are experiencing back or neck pain or symptoms that suggest a possible herniated disc, it is advisable to consult a specialist physician for diagnosis and appropriate treatment.
How Are Dislocated Vertebrae Put Back in Place?
Dislocated vertebrae in the spine are a common issue affecting many individuals. Patients often experience severe pain, tingling, and weakness in their limbs due to the instability of the vertebrae.
While surgery is the primary treatment for dislocated vertebrae, there are some methods that can help realign the vertebrae before resorting to surgery, including:
- Physical Therapy: This involves performing exercises that strengthen the muscles around the vertebrae to provide support and improve stability of the spine. Exercises may include stretching to alleviate pressure on the dislocated vertebrae. Physical therapy programs are tailored to the patient’s condition and guided by the therapist.
- Conservative Treatment: This involves maintaining proper body posture and avoiding activities that increase pressure on the vertebrae. The patient may need to use supportive equipment such as back braces to reduce pressure on the dislocated vertebrae.
- Medication: Pain-relieving medications can help alleviate the pain associated with dislocated vertebrae. Anti-inflammatory medications may be used to reduce inflammation in the affected area.
-